Consultation Skills
Gastrointestinal
Dyspepsia, GORD, constipation, diarrhoea, threadworm, IBS, haemorrhoids
Dyspepsia and GORD
Which of the following symptoms are specific to GORD only?
- Upper abdomen pain, described as a dull ache or discomfort
- Feeling bloated or heavy
- Burning sensation in the sternum area
- Acidic or sour taste in mouth
Red Flags
- Blood in vomit or stools
- Difficulty swallowing
- Unexplained weight loss
- Over 40 and first presentation
- Pain radiating down arm/cardiac association (Dyspepsia only)
Timescale for referral: 5-7 days
Product selection
-
PPI – both conditions
- Reduce acid production
- Long duration of action but also 2-3 day delay
- Up to 14 days treatment, >18
- Esomeprazole/omeprazole
-
Antacids – both conditions 抗酸剂
- Liquid or chewable tablets
- Neutralise excess acid - Effect short lived but immediate
- Liquids can be used in children
- Bisodol/Rennie/Mag trisilicate/Maalox etc
-
Alginates – mostly GORD 藻酸盐
- Liquid or chewable tablets
- Form a raft to protect the oesophagus and usually
- mixed with an antacid
- Effect short lived but immediate
- Usually, >12 years old
- Gaviscon
Constipation
Red flags
- Blood in stools
- Nausea and vomiting
- Abdominal pain
- Change sin bowel habit >2 weeks
Referral time:
- 2-3 days with OTC treatment
- 2 weeks with dietary advice
Product selection
- Osmotic laxatives 渗透性泻药
- Lactulose/Macrogol 乳果糖/聚乙二醇
- Draws water into the bowel
- Onset - 2-3 days
- Stimulant 兴奋剂
- Senna/Bisacodyl/Sodium picosulphate/glycerol supps 番泻叶/比沙可啶/硫酸钠/甘油栓剂
- Increase GIT motility (see MHRA guidance)
- Should not be used unless other laxatives and dietary modification are ineffective
- Stimulant laxatives should only ever be prescribed for children
- Onset – 8-12 hours
- Glycerol supps – 15-30 mins!!
- Bulk forming
- Ispaghula husk/methylcellulose 车前子壳/甲基纤维素
- Increase faecal mass and fluid
- Onset 12-36 hours
- Softening
- Docusate 多库酯
- Surfactant allows fluid to enter faeces + weak stimulant
- Onset – depends on route of admin
Diarrhoea
Red flags
- Blood/mucus/white fat like liquid in stools
- Change in bowel habit for more than 2 weeks
- Severe abdominal pain
Referral time:
- 1 day in children under 1
- 2 days in children under 3
- 3 days in older children and adults
Product selection
- Oral rehydration 口服补液盐
- Dioralyte
- Replaces fluid and electrolytes
- Does not stop diarrhoea
- Onset – immediately
- Loperamide 洛哌丁胺
- Reduces GIT motility and stops diarrhoea
- Onset – 2-4 hours but may need to take after each stool
Threadworm
Red flags
- Travel abroad
- Persistent/heavy infection
- Weight loss
- Appetite loss
- Insomnia
Referral time: Not resolved after 2nd dose
Product selection
- Mebendazole 甲苯咪唑
- Ovex liquid/chewable tablets
- Kills worms in the gut
- Onset – 1-2 days
- May need a 2nd dose in 2 weeks time
- Hygiene measures 卫生措施
- Prevent re-infestation
Irritable bowel syndrome (IBS)
Red flags
- Blood in stools
- White fat-like liquid in stools
- Unexpected weight loss
- Severe abdominal pain
- Undiagnosed IBS
Referral time: 1 week after OTC treatment if not resolved
NEEDS INITIAL DIAGNOSIS BY GP
Product selection
- Antispasmodic 解痉剂
- Mebeverine/peppermint oil 美贝维林/薄荷油
- Reduce cramping pain and spasms 减轻痉挛性疼痛和抽搐
- Hyoscine hydrobromide 氢溴酸东莨菪碱
- Smooth muscle relaxant
- Reduce cramping pain and spasms
- Laxatives 泻药
- To relive constipation
- Bulk forming/osmotic are the best for regular use
- Loperamide 洛哌丁胺
- To relieve diarrhoea
- Short term use only
Haemorrhoids (Piles)
Red flags
- Blood in stools
- Unexpected weight loss
- Severe abdominal pain when emptying bowels
Referral time: Up to 1 week
- Should be diagnosed by GP initially
- Need to keep bowel regular to prevent symptoms
Product selection
- Astringents 收敛剂
- Zinc oxide/bismuth/allantoin 氧化锌/铋/尿囊素
- Protective coat
- Anaesthetics 麻醉剂
- Lidocaine/benzocaine 利多卡因/苯佐卡因
- Temporary relief from pain/itching
- Corticosteroids
- Hydrocortisone
- Anti-inflammatory to reduce the size of the pile
- Antiseptics 抗菌剂
- Prevent infection
- Protectorants 保护剂
- Shark liver oil 鲨鱼肝油
- Coating to prevent pain and itching
Skin conditions
Eczema, contact dermatitis, acne vulgaris, burns and scalds, bites and stings
Eczema and Contact dermatitis
Eczema is a type of dermatitis!!
Red Flags
- Signs of infection
- Facial involvement
- Widespread area
Timescale for referral: 7 days if OTC product recommended
Product selection
- Emollients 润肤剂
- Moisturisers 保湿霜/soap substitutes/Bath/shower additives
- No active ingredient – paraffin based products 石蜡基产品
- Patient preference – creams/ointments
- Can be used by all (consider allergy e.g. lanolin 羊毛脂)
- Topical Corticosteroids
- Treat inflammation
- Hydrocortisone 1% cream (Hc45) 氢化可的松
- 10 years and over
- Clobetasone butyrate 0.05% cream (Eumovate) 丁酸氯倍他松
- 12 years and over
- Not licensed for use on:
- broken skin
- the face or ano-genital region
- Not to be used for more than 7 days
Acne
Red Flags
- Moderate to severe acne (see Core Concept)
Referral time: 6-8 weeks
Product selection
- Benzoyl peroxide 2.5%/5%/10% gel (Panoxyl Aquagel/Acnecide) 过氧化苯甲酰
- Antibacterial, anticomedogenic 抗致粉刺性 and keratolytic 角质溶解 properties
- Start with lowest strength and increase if necessary/tolerated
- Skin reddening/irritation possible especially at the start of treatment
- Can bleach clothes and bedding
- Nicotinamide 4% gel (Freederm) 烟酰胺: Mild anti-inflammatory action
Burns and scolds
Red flags
- Greater than patient’s palm size 手掌大小
- Burns on face or genitalia 生殖器
- Extensive blistering 大面积水疱形成
- Severe burn
- Pale/charred burn 浅色/焦黑烧痕
Referral time: Varies: 7-21 days/signs of infection
Product selection
- Keep cool: Burn gel/spray
- Keep clean: Use antiseptic spray/liquid
- Cover:
- Cling film 保鲜膜
- Low adherence dressing 低粘附性敷料
- hydrogel plaster 水凝胶绷带
- Pain relief
- Local aesthetic 局部麻醉剂
- Oral pain relief (paracetamol/ibuprofen)
Bites and Stings
Red flags
- Signs of infection
Referral time: 3-5 days
Product selection
- Antihistamines
- Prevent itching
- Mepyramine maleate cream (Anthisan) - > 2 yrs 马来酸甲哌胺
- Antihistamine tab/syrup: Chlorpheniramine (Piriton) - > 1 yr 氯苯那敏
- Topical corticosteroids – see previous
- Topical antiseptics 抗菌剂
- Topical anaesthetics 麻醉剂
- Benzocaine 苯佐卡因: Lanacane cream - > 12 yrs
Infectious skin conditions
Warts and verrucas, fungal skin infections, scabies, impetigo, herpes simplex/shingles
Warts and verrucae
Warts Verrucae Human papilloma Virus Human papilloma Virus Cauliflower like appearance On the soles of feet Mainly on hands Black capillaries visible
Red Flags
- Diabetes
- Change in size or colour
- Itching
- Bleeding
- Warts specifically on face or ano-gential area
- Multiple/widespread warts
Timescale for referral: 3 months (ensure realistic expectations of timescale)
Product selection
- Salicylic Acid (Bazuka, Salactol, Salactac)
- 2 years and over
- Protect the healthy surrounding skin (Vaseline) 凡士林
- Dimethyl Ether Propane (cryotherapy) 二甲醚丙烷(冷冻疗法)
- Over 4 years
- Requires precise application
Fungal Skin Infections
Red Flags
Athlete’s foot: (2 week referral)
- Signs of infection at wound site and systemic signs
- Diabetics
- Nail involvement 指甲受累
Fungal nail: (9-12 months referral)
- Signs of infection at wound site and systemic signs
- Diabetics
- More than 2 toenails affected
Ringworm: (4 weeks referral)
- Signs of infection at wound site and systemic signs
Sweat rash: (7 day referral)
- Signs of infection at wound site and systemic signs
Product Selection
Creams
- Terbinafine 1% cream (Lamisil) 特比萘芬 – FIRST LINE!!!
- Also available as a 1% cutaneous solution (Lamisil Once)
- Athletes foot and Jock itch only 仅限脚癣和股癣
- Clotrimazole 1% cream (Canesten AF) 克霉唑
- Ketoconazole 2% cream (Daktarin Gold) 酮康唑
- Also available as a 2% powder (Daktarin Aktiv powder) and a 0.16% spray powder (Daktarin Aktiv spray powder)
- Miconazole 2% cream (Daktarin) 咪康唑
- Available combined with hydrocortisone (Daktacort)
Powders
- Prevent reoccurrence – dust socks and shoes
- Daktarin powder
- Mycota powder
Nail Paints – fungal nail only
- Curanail (amorolifine 5% nail lacquer) 阿莫罗芬
- Over 18
- Once weekly
- 6-12 months treatment time
Scabies 疥疮
Red flags
- Signs of infection due to intensive itching
Timescale for referral: 2 weeks after first treatment
TREAT WHOLE HOUSEHOLD! CHECK APPROPRIATE FOR EACH MEMBER OF THE HOUSEHOLD!!
Product selection
-
Permethrin 5% Dermal cream (Lyclear Dermal cream) 氯菊酯
- Scabies and Crab Lice
-
Malathion 0.5% Liquid (Derbac-M) 马拉硫磷
- Head Lice, Scabies and Crab Lice 头虱、疥疮和阴虱
- Aqueous – suitable for asthmatics
Impetigo 脓疱疮
Red flags
- Eczema
- Signs of infection
Product selection
- Refer all cases – needs antibiotic treatment
- Crystacide (hydrogen peroxide 1%) – no evidence to support its use
Herpes Simplex / Shingles 单纯疱疹 / 带状疱疹
Red flags
Herpes simplex - (2 weeks)
- Signs of infection
- Lesions elsewhere on face or body
- Eyes affected
- Painless sores 无痛溃疡
Shingles – (4 weeks if only analgesia)
- Immunosuppression
- Eyes affected
Product selection
- Herpes
- Acicolvir (Zovirax) 阿昔洛韦(Acicolvir? Aciclovir? Acyclovir?)
- Adults and children
- Face and lips
- 5 times a day for 4 days (up to 10 days)
- Acicolvir (Zovirax) 阿昔洛韦(Acicolvir? Aciclovir? Acyclovir?)
- Shingles
- Refer
- Consider analgesia 镇痛
Respiratory
cough, cold, hay fever
Cough
Red Flags
- Chest pain
- Pain on inspiration
- Wheezing 喘息
- Shortness of breath
- Coughing up blood
Check for sputum – differential diagnosis 检查痰液
Timescale for referral: More than 3 weeks duration see GP
Product selection
-
Chesty/productive cough - Expectorants 有痰咳嗽 - 祛痰药
- Guaifenesin (Benylin chesty cough, Robitussin chesty cough) 愈创甘油醚
-
Demulcents 润喉
- Simple linctus
-
Dry/non productive cough
- Pholcodine (Galenphol, Covonia dry cough) 福尔可定
- Dextromethorphan (Benylin dry cough, Covonia original, Robitussin dry cough) 右美沙芬
- Codeine linctus – Adults - more historic (abuse potential) 可待因止咳糖浆
- Sedative antihistamines - diphenhydramine 苯海拉明
Colds
Red Flags
- Ear pain
- Muscle ache/chills/fatigue/dry cough and vulnerable group
- Pain on inspiration
- Wheezing
- Shortness of breath
Timescale for referral: 2 weeks
Product selection
-
Oral analgesics (+ caffeine/vit c)
- Paracetamol (Panadol, Calpol)
- Aspirin (Disprin, Beechams powders)
- NSAIDS i.e. Ibuprofen (Nurofen, Cuprofen)
-
Used in combination with opioids:
- Potential for addiction – 3 days max
- Codeine (co-codamol, Solpadeine Max) 可待因
- Dihydrocodeine (Paramol) 双氢可待因
-
Inhalations
- Eucalyptus oil/Vicks/Carvol/Olbas oil
-
Decongestants (systemic Vs topical)
- Be aware of contra indications!!
- Max 7 days treatment
- Pseudoephedrine/Phenylephrine – systemic 伪麻黄碱/苯肾上腺素
- Oxymetazoline/Xylometazoline - topical 羟甲唑啉/赛洛唑啉
-
Combination products (analgesic/decongestant/cough)
- E.g. night nurse/day nurse/covonia cold and flu
- These can be useful – but check:
- That all ingredients are needed and appropriate
- Drowsiness s/e’s with antihistamine
Hay fever (seasonal allergic rhinitis)
Red Flags
- Unilateral nasal blockage 单侧鼻塞
- Muscle ache/chills/fatigue/dry cough and vulnerable group 肌肉酸痛/畏寒/疲劳/干咳以及易感人群
Timescale for referral: 2 weeks
Product selection
- Oral antihistamines 口服抗组胺药
- Non drowsy – adults and children
- Loratadine tabs 6+/syrup 2+ 氯雷他定
- Cetirizine tabs 12+/syrup 2+ 西替利嗪
- Acrivastine capsules 12+ 阿克拉维斯汀
- Drowsy - adults and children
- Chlorphenamine tabs 6+/syrup 1+ 氯苯那敏
- Non drowsy – adults and children
- Steroid Nasal sprays 类固醇鼻喷雾剂
- Over 18’s only
- Most effective for nasal symptoms, not immediate action
- Beclometasone 倍氯米松
- Fluticasone 氟替卡松
- Budesonide 布地奈德
- Mometasone 莫米松
- Triamcinolone 曲安奈德
- Eye drops 眼药水
- Sodium cromoglicate 6+ 色甘酸钠
- Decongestant tablets 减充血剂片剂
- Pseudoephedrine tabs (Remember contra-indications!)
- Other nasal sprays
- Decongestant nasal sprays 减充血剂鼻喷剂
- Oxymetazoline/Xylometazoline Max 7 days – rebound congestion
- Protectants 鼻腔保护剂
- Prevalin
- Saline 盐水
- Decongestant nasal sprays 减充血剂鼻喷剂
Core Concept - Immunity and Infection
LECTURE 7: 01 Core Concept 5 - Interaction of Pathogens (病原体相互作用)
Lecturer: Gavin Humphreys
1. Introduction & Key Definitions
Bacterial Abundance
- Global Scale: There are estimated to be $10^{30}$ bacterial cells on Earth.
- Human Scale: Bacterial cells in/on the human body outnumber eukaryotic cells (真核细胞) by a ratio of approximately 1.3 : 1.
- Location: The majority reside in the gut, but they also colonize the skin, nasal cavity, respiratory tract, etc.
Commensal vs. Pathogen
- Commensal Microbiota (共生菌群): Bacteria that normally live on/in a healthy host without causing harm.
- Functions/Benefits:
- Immune Development: Colonization from birth helps train the immune system.
- Colonisation Resistance (定植抗力): They occupy space and consume nutrients, preventing pathogens from establishing a stronghold.
- Metabolic Organ: They break down complex indigestible carbohydrates that humans cannot digest.
- Functions/Benefits:
- Opportunistic Pathogen (条件致病菌 / 机会致病菌): Commensals that cause disease when the host’s immune system is compromised or when they enter a sterile site.
- Obligate Human Pathogen (专性人类致病菌): Microorganisms that must cause disease to be transmitted and survive (e.g., Neisseria gonorrhoeae). They generally do not survive well outside the host.
Immunocompromised States (免疫功能低下状态)
Opportunistic infections occur when host defenses are breached:
- Damage to Epithelia (上皮损伤): Cuts, surgical wounds, eczema, burns.
- Disruption of Commensals: Overuse of antibiotics (e.g., leading to C. difficile).
- Immune Impairment: Flu/RSV infections, HIV/AIDS, chemotherapy.
- Foreign Devices: Catheters (导管), prosthetic joints (no blood supply/immune presence, prone to biofilm (生物被膜) formation).
2. Transmission of Infection (Epidemiology / 流行病学)
Bacteria spread via various routes. These routes often overlap.
Horizontal Transmission (水平传播)
(Person-to-Person / Environment-to-Person)
- Aerosol/Airborne (气溶胶/空气传播): Droplets from coughing/sneezing (e.g., Influenza, COVID-19).
- Small droplets: Stay suspended in air, travel through ventilation.
- Large droplets: Fall within ~2 meters, contaminating surfaces.
- Direct Contact: Skin-to-skin contact (e.g., unwashed hands of healthcare workers).
- Fomite (污染物 / 非生物媒介): Inanimate objects that transfer infection (e.g., mobile phones, keyboards, door handles).
- Vehicle (媒介物): Contaminated food or water.
- Vector (生物媒介 / 载体): Living organisms (arthropods) that transmit disease (e.g., mosquitoes).
Vertical Transmission (垂直传播)
(Parent-to-Child)
- Via Placenta (胎盘): During pregnancy.
- During Birth: Contact with vaginal canal (e.g., Gonorrhea conjunctivitis).
- Via Breast Milk.
3. Virulence Factors (毒力因子)
To cause disease, bacteria produce Virulence Factors. These are strategies to:
- Promote Colonisation & Invasion (定植与侵袭).
- Cause Host Damage (Toxicity / 毒性).
- Enable Immune Evasion (免疫逃逸).
A. Adhesion & Motility (黏附与运动)
The first step in infection is attaching to a surface to prevent being washed away.
- Fimbriae / Pili (菌毛):
- Short, hair-like protein appendages anchored to the outer membrane.
- Function:
- Intimate Attachment: Adhesins (黏附素) at the tip bind specific host receptors.
- Twitching Motility (蹭行运动): Extend, attach, and retract to drag the bacteria along a surface (“force-driven contraction”).
- Biofilm Formation: Aid in aggregation.
- Flagella (鞭毛):
- Long, rigid, corkscrew-like structures.
- Function: Motility (movement). Powered by a proton motor to rotate.
- Microbial Taxis (趋性): Movement towards nutrients or away from danger (toxins/UV).
B. Immune Evasion: Capsules (免疫逃逸:荚膜)
- Structure: A polysaccharide (多糖) layer surrounding the bacterial cell.
- Importance: Critical for invasive infections (survival in the blood, e.g., meningitis, pneumonia). Without a capsule, these bacteria are easily cleared.
- Mechanisms of Evasion:
- Charge Effect: Capsules often have a high negative charge. Since phagocytes (吞噬细胞) are also negatively charged, electrostatic repulsion prevents phagocytosis.
- Mimicry (抗原伪装): The capsule composition mimics host tissue (e.g., Hyaluronic acid / 透明质酸), masking the bacteria from the immune system. (It coats itself in what the immune system thinks is host tissue [connective tissue], so it doesn’t recognize it as an invading pathogen).
Case Study: Neisseria meningitidis (Meningitis / 脑膜炎)
- Virulence: The capsule is the critical factor allowing survival in the blood (septicaemia / 败血症) and crossing the blood-brain barrier (meningitis).
- Capsule Serotype B: Mimics host tissue (NCAM). This made vaccine development difficult (took ~30 years) because the immune system does not recognize it as foreign.
- Clinical Sign: Non-blanching rash (压之不褪色的皮疹) caused by bacteria damaging capillaries and leaking blood.
4. Bacterial Toxins (Host Damage)
Bacteria damage the host to obtain nutrients or spread.
1. Endotoxins (内毒素) - Lipopolysaccharide (LPS)
- Origin: Innate part of the Gram-negative bacterial outer membrane (specifically Lipid A, a part of Lipopolysaccharide).
- Release: Released only when the bacterial cell dies or lyses.
- Mechanism: Not site-specific.
- Effect: Highly immunogenic. Triggers a massive, uncontrolled inflammatory response (Cytokine storm / 细胞因子风暴, Complement activation).
- Outcome: Can lead to Septicemia / Sepsis (脓毒症).
2. Exotoxins (外毒素)
- Origin: Proteins specifically produced and secreted by living bacteria (both Gram+ and Gram-).
- Mechanism: Site-specific; they travel through the blood to target specific distal organs or cells.
- Examples:
- Scalded Skin Syndrome (葡萄球菌烫伤样皮肤综合征): Toxin produced in the umbilicus/nose enters blood, travels to skin, and cleaves desmoglein (skin glue / 桥粒芯糖蛋白), causing skin to peel off.
Case Study: Pneumolysin (Streptococcus pneumoniae)
A pore-forming exotoxin (成孔毒素) targeting cholesterol in host cell membranes.
- Target: Respiratory tract (causes Pneumonia).
- Action 1: Immunosuppressive (Early stage/Low conc):
- Attacks the cholesterol receptor, and it will open up a pore randomly in membrane. Inhibits the mucociliary escalator (黏液纤毛清除系统) (stops cilia beating), preventing clearance of bacteria.
- Causes apoptosis (cell death) of resident macrophages.
- Action 2: Pro-inflammatory (Late stage/High conc):
- Recruits Neutrophils (中性粒细胞) to the lungs.
- While this sounds like a defense, the neutrophils release enzymes that cause massive tissue damage (consolidation / 实变 in lungs), allowing bacteria to proliferate further.
- Symptoms: Fever, malaise, dyspnoea (breathlessness / 呼吸困难), productive cough, crackles.
Summary Table: Endotoxin vs. Exotoxin (内毒素与外毒素对比)
| Feature | Endotoxin (内毒素) | Exotoxin (外毒素) |
|---|---|---|
| Source | Gram-negative bacteria only | Gram-positive & Gram-negative |
| Location | Part of cell wall (LPS / Lipid A) | Secreted from the cell |
| Release | Upon cell death/lysis | Produced by living cells |
| Specificity | Non-specific (Systemic inflammation) | Highly specific targets (e.g., nerves, skin) |
| Heat Stability | Heat stable (耐热) | Heat labile (不耐热, usually proteins) |
| Example | Meningococcal Septicemia | Pneumolysin, Tetanus, Botulinum |
LECTURE9 01 Core Concept 7 Overview of Immunity
Lecturer: Dr. Costas Demonacos
1. Introduction to the Immune System (免疫系统简介)
Role & Function
The immune system’s primary role is to provide defense (防御) against various pathogens (bacteria, viruses, parasites, fungi).
- Beneficial (有益):
- Protection from Invaders (防御外来入侵).
- Elimination of Altered Self (e.g., cancer cells) (清除自身变异细胞).
- Detrimental (有害/副作用):
- Discomfort (Inflammation) (不适/炎症).
- Damage to self (Autoimmunity) (自身免疫损伤).
Two Major Elements
| Feature | Innate Immune System (先天性免疫系统) | Adaptive Immune System (适应性免疫系统) |
|---|---|---|
| Response Time | Rapidly evoked (First line of defense) (快速响应) | Slow activation (慢速激活) |
| Specificity | Non-specific (非特异性) | Highly specific (高度特异性) |
| Memory | No memory (无记忆) | Immunological memory (免疫记忆) |
| Development | Present from birth (与生俱来) | Developed/Refined over time (后天获得) |
2. Cells of the Immune System (免疫细胞)
Immune cells originate from Hematopoietic stem cells (造血干细胞) and differentiate into two main lineages: Myeloid (髓系) and Lymphoid (淋巴系).
A. Myeloid Lineage (Innate Immunity mostly) (髓系细胞 - 主要负责先天免疫)
- Antigen Presenting Cells (APCs) (抗原提呈细胞):
- Function: Capture, process, and present antigens to adaptive immune cells (T cells). This bridges innate and adaptive immunity.
- Macrophages (巨噬细胞): Phagocytose (吞噬) pathogens, break them down, and present peptides.
- Dendritic Cells (DCs) (树突状细胞): “Professional” APCs. Located in tissues (skin, mucosa), capture antigens, and transport them to lymph nodes to activate T cells.
- B cells as well that can be antigen presenting cells
- Granulocytes (粒细胞):
- Neutrophils (中性粒细胞):
- Main defense against rapidly dividing bacteria (快速分裂的细菌).
- First to migrate to infection sites (Chemotaxis).
- Mechanism: Phagocytosis and destruction.
- Basophils (嗜碱性粒细胞):
- Produce different granules which contain several chemicals that attack foreign microorganisms, the contents of the granules are enzymes and proteins and so on which can then eliminate microorganisms.
- Release Histamine (组胺).
- Active in allergic reactions (过敏反应).
- Eosinophils (嗜酸性粒细胞):
- Similar to basopils
- Release toxins to kill parasites (worms/protozoa) (寄生虫).
- Involved in allergic asthma.
- Release Histamine.
- Mast Cells (肥大细胞):
- Concentrated under body surfaces (skin, mucosa).
- Release factors causing vasodilation (血管扩张) and increased permeability (inflammation).
- Neutrophils (中性粒细胞):
- Natural Killer (NK) Cells (自然杀伤细胞):
- Note: Part of the Innate system despite lymphoid origin.
- Target: Virus-infected cells (病毒感染细胞) and Cancer cells (癌细胞).
- Mechanism: Recognize cells with low MHC Class I (主要组织相容性复合体 I类) expression. (Healthy cells inhibit NK cells via MHC I; infected/tumor cells often lose MHC I to hide, thus triggering NK killing).
- the natural killer cells have two receptors, the activating receptor and the repressive receptor.
| Component of innate immunity | Main mechanisms of action |
|---|---|
| Mast cells (concentrated under the body surfaces) | Release factors which increase blood flow and vascular permeability bringing components of immunity to the site of infection |
| Neutrophils and macrophages (phagocytes) | Engulf (phagocytose) and destroy micro-organisms |
| Eosinophils | Secrete factors which kill protozoa and worms |
| Natural killer cells | Destroy virus infected cells |
| Cytokines - interferon | Toxic to viruses |
B. Lymphoid Lineage (Adaptive Immunity mostly) (淋巴系细胞 - 主要负责适应性免疫)
- T Lymphocytes (T Cells) (T 淋巴细胞):
- CD4+ T Helper Cells ($T_H$) (辅助性 T 细胞):
- Recognize antigen on MHC Class II (MHC II类分子) (Macrophages, dendritic cells and B cells
which are antigen presenting cells
present antigen on MHC Class II). - Th1: Stimulate Cell-Mediated Immunity (CMI) (细胞免疫).
- Th2: Stimulate B cells to produce antibodies (Humoral Immunity) (体液免疫).
- Recognize antigen on MHC Class II (MHC II类分子) (Macrophages, dendritic cells and B cells
- CD8+ Cytotoxic T Cells ($T_C$) (细胞毒性 T 细胞):
- Recognize antigen on MHC Class I (MHC I类分子) (present on all nucleated cells).
- Directly kill infected/abnormal cells by producing enzymes and molecules, chemicals that are cytotoxic (Cytotoxicity).
- CD4+ T Helper Cells ($T_H$) (辅助性 T 细胞):
- B Lymphocytes (B Cells) (B 淋巴细胞):
- Differentiate into Plasma Cells (浆细胞).
- Produce Antibodies (Immunoglobulins, Ig) (抗体/免疫球蛋白).
3. Antibody Structure & Function (抗体结构与功能)
- Structure: Y-shaped.
- Fab region (Amino terminal): Recognizes and binds to specific Antigen (抗原).
- Fc region (Carboxy terminal): Binds to receptors on immune cells (recruitment).
- The amino terminal end, the top part of the antibody, recognizes the antigen whereas the bottom part, the carboxy terminal end, binds to receptors that exist on cells of the immune system.
- Functions:
- Opsonisation (识别作用): Coating pathogens to make them “visible” and easier for phagocytes to eat.
- Neutralisation (中和作用): Binding to toxins or viruses to prevent them from entering/damaging cells.
- Complement Activation (补体激活): Triggering the complement cascade to form a “tube” (Membrane Attack Complex) that punches holes in bacteria.
- ADCC (Antibody-Dependent Cellular Cytotoxicity) (抗体依赖性细胞介导的细胞毒性): Recruiting cells (like NK cells) to kill targets bound by antibodies.
- Classes of Immunoglobulins:
- IgM: First produced, produced from activated B lymphocytes.
- IgG: Main antibody in circulation; long-term immunity; produced by B cells that are differentiated by the interferon gamma (γ干扰素).
- IgA: Mucosal immunity; passed to infants via breast milk.
- IgE: Involved in Allergy (过敏) and parasitic infections.
Immunological Memory (免疫记忆)
- Primary Response (初次应答): Slow (lag phase ~12 days), lower magnitude.
- Secondary Response (二次应答): Fast (lag phase ~4 days), much stronger (robust), due to Memory B/T cells.
4. Hypersensitivity (Allergy) (超敏反应/过敏)
Hypersensitivity is an inappropriate immune response to benign antigens (allergens).
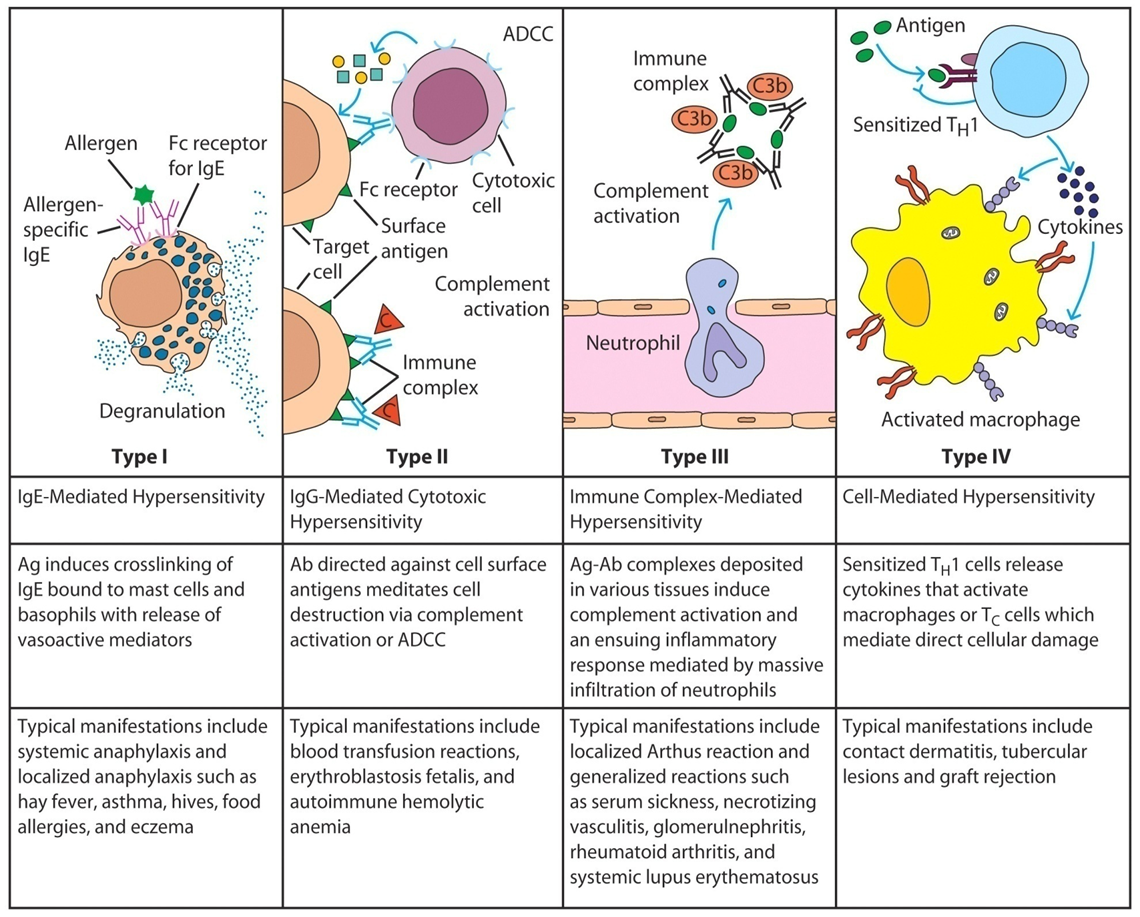
Type I Hypersensitivity (IgE-Mediated) (I型超敏反应)

- Mechanism:
- First exposure to allergen $\rightarrow$ Production of IgE.
- IgE binds to Fc receptors on Mast Cells (Sensitization).
- Subsequent exposure $\rightarrow$ Allergen cross-links IgE on mast cells.
- Degranulation (脱颗粒): Massive release of Histamine (组胺) and other vasoactive amines.
- Symptoms: Vasodilation, itching, bronchoconstriction (Asthma), systemic anaphylaxis.
- the production of IgE stimulates the mast cells to produce those allergens, which those vasoactive amines, which now cause all these undesirable effects on our body.
- allergies to pollen (花粉过敏)
Treatment Strategy
- Antihistamines (抗组胺药): Block histamine receptors to prevent symptoms (do not stop the release, just the effect).
Summary Table: Innate vs. Adaptive Cells
| Cell Type | Lineage | System | Main Function |
|---|---|---|---|
| Neutrophil | Myeloid | Innate | Phagocytosis (Bacteria) |
| Macrophage | Myeloid | Innate | Phagocytosis + Antigen Presentation |
| Dendritic Cell | Myeloid | Innate | Professional Antigen Presentation |
| NK Cell | Lymphoid | Innate | Kill virus/cancer cells (low MHC I) |
| B Cell | Lymphoid | Adaptive | Produce Antibodies (Humoral) |
| T Helper (CD4) | Lymphoid | Adaptive | Coordinate response (Cytokines) |
| Cytotoxic T (CD8) | Lymphoid | Adaptive | Kill infected cells (Cellular) |
LECTURE11 01 Core Concept 9 Antimicrobial Mechanisms
Lecturer: Richard Bryce
1. Introduction to Microorganisms & Selective Toxicity
Microbes & Microbiota
- Microbiota (微生物群): Microbes living in and around the body (e.g., intestines). 95% located in the GI tract.
- Microbiome (微生物组): The genetic material of all these micro-organisms.
- Pathogenic (致病的): Causing disease vs. Beneficial (Beneficial flora).
Selective Inhibition (选择性抑制)
To safely treat infections, drugs must target structures or processes unique to bacteria (prokaryotes) that are absent or different in humans (eukaryotes).
Key Bacterial Targets:
- Outside:
- Cell Wall (细胞壁): Peptidoglycan (肽聚糖) structure.
- Cell Membrane (细胞膜): Plasma membrane.
- Inside:
- Circular DNA (环状 DNA): And plasmids.
- Ribosomes (核糖体): 70S (50S + 30S), unlike human 80S.
- Metabolic Pathways (代谢途径): Unique enzymes (e.g., folate synthesis).
Gram-positive vs. Gram-negative Bacteria
- Gram-positive (革兰氏阳性菌): Thick peptidoglycan layer, no outer membrane.
- Gram-negative (革兰氏阴性菌): Thin peptidoglycan layer, has an Outer Membrane (外膜) containing Lipopolysaccharides (LPS).
2. Target #1: Bacterial DNA (细菌 DNA)
The Problem: DNA Compaction
- Bacterial DNA is circular and very long (~1300 μm). It must fit into a tiny cell.
- Supercoiling (超螺旋): The DNA double helix is twisted into a superhelix to compact it.
- Negative Supercoiling (负超螺旋): Left-handed coiling. Loosens strands for replication/transcription. Most common.
- Positive Supercoiling (正超螺旋): Right-handed. Found in thermophiles to prevent denaturation.
The Enzymes: Topoisomerases (拓扑异构酶)
- DNA Gyrase (DNA 促旋酶): Introduces negative supercoils. Essential in Gram-negative bacteria.
- Topoisomerase IV (拓扑异构酶 IV): Essential in Gram-positive bacteria.
- Mechanism: Cuts one DNA region $\rightarrow$ Passes another region through the break $\rightarrow$ Reseals the break.
Drug Class 1: Quinolones (喹诺酮类)
These are DNA Gyrase Inhibitors.
- 1st Generation: Nalidixic acid (萘啶酸) (1962).
- Mainly active against Gram-negative.
- Used for UTIs (Urinary Tract Infections).
- Bacteriocidal (杀菌的): Irreversible inhibition.
- 2nd Generation (Fluoroquinolones): Ciprofloxacin (环丙沙星) (1980).
- Fluorine atom added (Fluoro-).
- Increased Gram-positive activity.
- 3rd Generation: Levofloxacin (左氧氟沙星) (1993).
- Active against Streptococci (e.g., S. pneumoniae).
- Broad spectrum (广谱).
Drug Class 2: Nitroimidazoles (硝基咪唑类)
- Example: Metronidazole (甲硝唑).
- Mechanism (DNA Strand Breaking):
- Requires Anaerobic environment (厌氧环境) to activate.
- Nitro group ($-NO_2$) is reduced by bacterial electron transport to a Nitro radical anion.
- Forms a toxic imidazole radical that extracts hydrogen from DNA, causing strand breaks (“Bactericidal Fireworks”).
- Clinical Use: Anaerobic infections (e.g., C. difficile, Bacterial Vaginosis) and Protozoa.
- Side Effect: Alcohol intolerance (Disulfiram-like reaction).
3. Target #2: Protein Synthesis (Ribosomes)
Key Difference: Bacteria use 70S Ribosomes (30S small subunit + 50S large subunit). Humans use 80S.
- Inhibition is usually Bacteriostatic (抑菌的) (stops growth, doesn’t kill).
The Translation Process & Drug Targets
- Initiation (起始): Subunits bind mRNA.
- Subunits bind with mRNA “instructions” in middle (read from 5’ to 3’). Inhibitor: Oxazolidinones (e.g., Linezolid). Binds 50S, prevents formation of the initiation complex (70S).
- Elongation (延伸):
- tRNA brings amino acid (encoded by codon) to A site. Inhibitor: Tetracyclines.
- Peptide bond formation (Peptidyl transferase). Growing peptide chain at P site then added to tRNA in A site. Inhibitor: Chloramphenicol.
- Deacylated tRNA exits from P site via E site
- Peptidyl-tRNA moves from A to P site (translocation). Inhibitor: Macrolides.
- Termination (终止).
- Process terminates (stop codon) and subunits dissociate.
Drug Classes
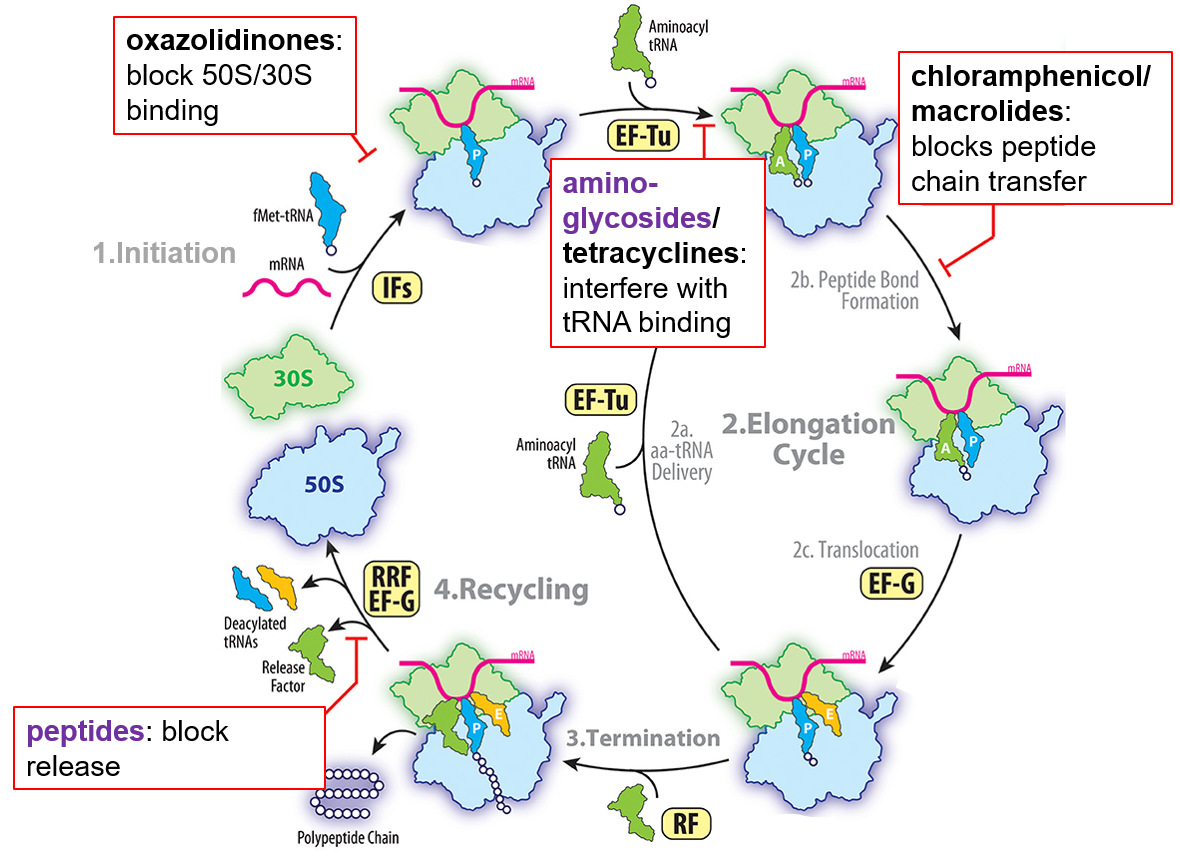
A. Oxazolidinones (噁唑烷酮类)
- Example: Linezolid (利奈唑胺).
- Action: Binds 50S subunit. Blocks initiation.
- Use: “Reserve” antibiotic for multi-resistant Gram-positive bacteria (e.g., MRSA, VRE).

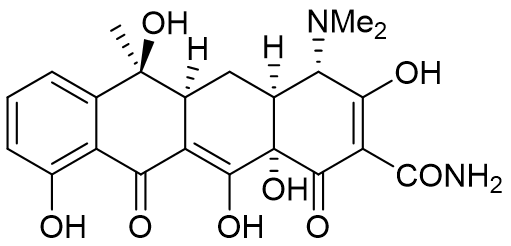
B. Tetracyclines (四环素类)
- Example: Tetracycline.
- Action: Binds 30S subunit. Blocks aminoacyl-tRNA binding (A-site).
- Use: Acne, Lyme disease, Malaria.
- Contraindication: Children (Stains developing tooth enamel/bones).
- Widespread resistance (vet use, feedstock additive)
C. Macrolides (大环内酯类)
- Example: Erythromycin (红霉素).
- Action: Binds 50S subunit near the exit tunnel (near peptidyl transferase centre). Blocks Translocation (易位) and peptide exit.
- Use: Gram-positive infections (Penicillin-allergic patients), Respiratory infections.
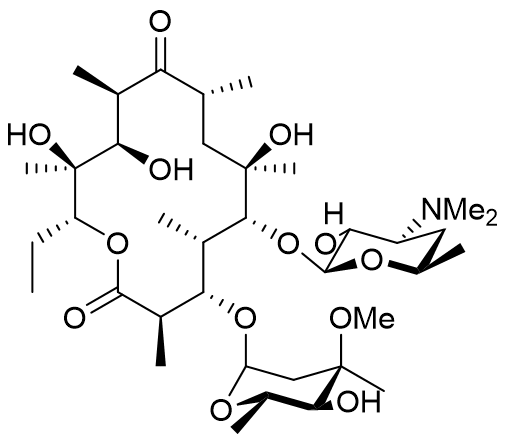
D. Chloramphenicol (氯霉素)
-
Action: Binds 50S subunit. Also inhibits Peptidyl Transferase (肽基转移酶) (peptide bond formation).
- Note: Competes with Macrolides (cannot use together).
-
Use: Eye/Ear infections (drops), Typhoid.
-
Toxicity: Bone marrow toxicity (avoid in infants - “Grey baby syndrome”).
4. Target #3: Metabolism (Folate Pathway)
Why Folate? Folate (Vitamin B9) is essential for synthesizing DNA bases (thymidine).
- Humans: Absorb folate from diet (cannot synthesize it).
- Bacteria: Must synthesize folate de novo (cannot absorb it). Selective Target!
- key enzyme = dihydrofolate reductase (DHFR)
- common to humans and bacteria, but differences in amino acid sequence and structure
- can be also used to target cancer (human DHFR), malaria (P. falciparum DHFR)


The Pathway & Inhibitors (Antimetabolites - 抗代谢物)
- Step 1: PABA $\rightarrow$ Dihydropteroate
- Enzyme: DHPS (Dihydropteroate synthase). Unique to bacteria.
- Inhibitor: Sulfonamides (Sulfa drugs) e.g., Sulfamethoxazole.
- Mechanism: Mimics the substrate PABA (p-aminobenzoic acid). Competitive inhibition.
- SAR (Structure-Activity Relationship): Requires aromatic ring with para-amino group ($p-NH_2$). Secondary sulphonamide group ($pK_a$ 5-8) improves activity.
- Step 2: Dihydrofolate $\rightarrow$ Tetrahydrofolate
- Enzyme: DHFR (Dihydrofolate reductase). Present in humans too, but bacterial enzyme is structurally different.
- Inhibitor: Trimethoprim (甲氧苄啶).
- Mechanism: Mimics the Pteridine ring (蝶啶环) of folate. 100,000x more selective for bacterial DHFR. Used for UTIs in combination with other antibiotics e.g., SEPTRIN (see later).
- Inhibitor: Methotrexate (MTX) (甲氨蝶呤).
- Also targets human DHFR so mainly used against cancer and rheumatoid arthritis.
Combination Therapy: Co-trimoxazole (复方新诺明/Septrim)
- Combination: Sulfamethoxazole + Trimethoprim.
- Concept: Sequential Blocking (序贯阻断). Hits multiple enzymes in the same pathway.
- Benefit: Synergistic effect, lower doses required, reduces resistance.
- Use: UTIs, Pneumocystis pneumonia (in AIDS).
Summary Table: Drug Mechanisms
| Drug Class | Target Site | Specific Mechanism | Effect |
|---|---|---|---|
| Quinolones | DNA Gyrase / Topo IV | Prevents supercoiling (DNA replication) | Bacteriocidal |
| Nitroimidazoles | DNA Structure | Free radicals break DNA strands | Bacteriocidal |
| Oxazolidinones | 50S Ribosome | Prevents Initiation complex | Bacteriostatic |
| Tetracyclines | 30S Ribosome | Blocks tRNA binding (A-site) | Bacteriostatic |
| Macrolides | 50S Ribosome | Blocks Translocation / Exit tunnel | Bacteriostatic |
| Chloramphenicol | 50S Ribosome | Inhibits Peptidyl transferase | Bacteriostatic |
| Sulfonamides | DHPS Enzyme | Mimics PABA (Folate synthesis) | Bacteriostatic |
| Trimethoprim | DHFR | Mimics the Pteridine ring of folate | Bacteriostatic |
LECTURE12 01 Core Concept 10 Beta-Lactam agents
Lecturer: Richard Bryce
1. Introduction & Targets (引言与靶点)
Following the previous lecture on intracellular targets (DNA, Ribosomes), this lecture focuses on external targets unique to bacteria:
- Cell Wall (细胞壁): Synthesis inhibition.
- Cell Membrane (细胞膜): Disruption.
2. Target #4: Bacterial Cell Wall Synthesis (细菌细胞壁合成)
The Target: Peptidoglycan (肽聚糖)
- Function: Provides mechanical strength to withstand high internal osmotic pressure (渗透压). Without it, the cell absorbs water and bursts (lysis/溶菌).
- Structure: A polymer mesh (“chicken wire”).
- Glycan chains (聚糖链): Alternating sugars NAM (N-acetylmuramic acid) and NAG (N-acetylglucosamine).
- Peptide cross-links (肽交联): Short peptides linking the sugar chains.
Gram-Positive vs. Gram-Negative (革兰氏阳性 vs 阴性)
- Gram-Positive (+): Thick peptidoglycan layer on the outside. Retains purple stain.
- Gram-Negative (-): Thin peptidoglycan layer sandwiched between an Inner Membrane and an Outer Membrane (外膜). Drugs must pass through Porins (孔蛋白) to reach the cell wall.
The Enzyme: Transpeptidase (转肽酶)
- Also known as Penicillin Binding Protein (PBP).
- Mechanism: It catalyzes the cross-linking of peptide chains.
- It connects D-Alanine to DAP (Diaminopimelic acid).
- Active Site: Contains a Serine (丝氨酸) residue that attacks the peptide to form the bond.
3. Beta-Lactam Antibiotics: Penicillins (青霉素类)
Structure
- Beta-Lactam Ring ($\beta$-内酰胺环): A 4-membered cyclic amide. Highly strained (90° bond angles) and reactive.
- Thiazolidine Ring (噻唑烷环): 5-membered sulfur-containing ring.
- Key Features: Cis-protons, carboxylic acid, amide side chain.
Mechanism of Action (作用机制)
- Irreversible Inhibition (不可逆抑制): The Beta-lactam ring mimics the D-Ala-D-Ala substrate.
- The Transpeptidase attacks the beta-lactam ring instead of the cell wall peptide.
- The ring opens and forms a stable covalent bond (共价键) with the enzyme’s Serine residue.
- The enzyme is permanently disabled $\rightarrow$ No cross-linking $\rightarrow$ Cell wall weakens $\rightarrow$ Cell lysis (Bactericidal/杀菌).
Penicillin G (The Original)
- Limitations:
- Acid Sensitivity (酸敏感性): Destroyed by stomach acid (cannot be taken orally).
- Beta-Lactamase Sensitivity ($\beta$-内酰胺酶敏感性): Bacteria produce enzymes (Beta-lactamases) that break the ring.
- Narrow Spectrum (窄谱): Active mainly against Gram +ve; ineffective against Staphylococci.
Drug Development (Solving the Problems)
1. Solving Acid Sensitivity (Oral Administration)
- Problem: The side chain carbonyl attacks the beta-lactam ring in acid.
- Solution: Add an Electron-Withdrawing Group (吸电子基团) (e.g., $NH_2$) to the side chain.
- Drug: Ampicillin (氨苄西林) / Amoxicillin (阿莫西林).
- Acid stable (can be taken orally).
2. Solving Beta-Lactamase Resistance (Enzyme Resistance)
- Problem: Bacteria break the drug before it works.
- Solution: Add a Bulky Side Chain (大体积侧链) (Steric Shield) to block the Beta-lactamase from binding.
- Drugs:
- Methicillin (甲氧西林): Acid sensitive (must be injected).
- Oxacillin (苯唑西林) / Flucloxacillin: Acid stable & Beta-lactamase resistant.
- Note: MRSA (Methicillin-Resistant S. aureus) has mutated transpeptidases that don’t bind these drugs.
3. Increasing Spectrum (Broad Spectrum)
- Hydrophobic side chains: Good for Gram-positive.
- Hydrophilic side chains: Better for Gram-negative (pass through porins).
- Drug: Carbenicillin (羧苄西林).
- Has a hydrophilic carboxyl group. Active against both Gram +ve and Gram -ve (e.g., Pseudomonas).
4. Other Beta-Lactams (其他 $\beta$-内酰胺类)
Cephalosporins (头孢菌素)
- Structure: 6-membered dihydrothiazine ring (instead of 5-membered thiazolidine).
- Generations (1st - 4th): Developed to improve stability and Gram-negative activity.
Beta-Lactamase Inhibitors (酶抑制剂)
- Clavulanic Acid (克拉维酸):
- Structure looks like penicillin but has no antibacterial activity itself.
- Mechanism: “Suicide inhibitor”. It permanently binds to and inactivates Beta-lactamases.
- Usage: Combined with Amoxicillin (e.g., Augmentin / Co-amoxiclav). The Clavulanic acid sacrifices itself so Amoxicillin can kill the bacteria.
5. Non-Beta-Lactam Cell Wall Inhibitors
Vancomycin (万古霉素)
- Structure: Huge Glycopeptide (Sugar + Peptide).
- Mechanism:
- Does NOT bind to the enzyme (transpeptidase).
- Binds to the Substrate (底物) (the D-Ala-D-Ala tail of the cell wall peptide) via Hydrogen bonds.
- Acts as a physical barrier (“Samson in the temple”), preventing cross-linking.
- Use: Serious Gram-positive infections (e.g., MRSA, C. difficile). Too big to pass Gram-negative outer membrane.
- Resistance: VRE/VRSA (Bacteria change the peptide from D-Ala-D-Ala to D-Ala-D-Lactate, so Vancomycin can’t bind).
6. Target #5: Cell Membrane (细胞膜)
Gramicidin A (短杆菌肽 A)
- Structure: Peptide that coils into a helix.
- Mechanism: Two molecules dimerize in the membrane to form an Ion Channel (离子通道).
- Effect: Uncontrolled flow of ions (e.g., $K^+, Na^+$) destroys ion gradients $\rightarrow$ Cell death.
- Toxicity: Can affect human cells too. Used only Topically (局部使用) (e.g., eye drops, creams).
Summary Table
| Drug Class | Target | Mechanism | Effect |
|---|---|---|---|
| Penicillins | Transpeptidase | Covalent binding to enzyme | Bactericidal |
| Cephalosporins | Transpeptidase | Covalent binding to enzyme | Bactericidal |
| Clavulanic Acid | Beta-Lactamase | Inhibits the enzyme that breaks penicillins | Protective |
| Vancomycin | D-Ala-D-Ala (Substrate) | Physically blocks cross-linking | Bactericidal |
| Gramicidin A | Cell Membrane | Forms ion pores | Bactericidal |
LECTURE19 01 Core Concept 16 Antimicrobial resistance
Lecturer: Andrew McBain (Transcript indicates guest delivery or recording)
1. Introduction & Historical Context (引言与历史背景)
The “Post-Antibiotic Era” (后抗生素时代)
- Pre-Antibiotic Era (1900): The leading causes of death were infectious diseases (e.g., influenza, pneumonia, tuberculosis, gastroenteritis). Life expectancy was lower.
- Antibiotic Era (Present/Recent): Major causes of death shifted to non-communicable diseases (e.g., heart disease, cancer, stroke).
- Current Threat: We are approaching a “post-antibiotic era” where common infections could kill again due to resistance. Patients are already dying from infections with no suitable antibiotic treatment options.
Defining Resistance (耐药性的定义)
- Definition: The acquired ability (获得性能力) of a microorganism to resist the effects of a chemotherapeutic agent to which it is normally sensitive.
- Crucial Concept: It is the microbe (microorganism) that becomes resistant, NOT the patient.
- Note: Do not say “The patient became resistant to penicillin.” Say “The bacteria infecting the patient became resistant.”
2. Classifications of Resistance (耐药性的分类)
1. Intrinsic / Natural Resistance (固有/天然耐药)
The organism is naturally resistant without needing genetic mutation.
- Examples:
- Lactobacilli in yoghurt are intrinsically resistant to Vancomycin (not clinically problematic).
- Gram-negative bacteria are intrinsically resistant to antibiotics that cannot cross their outer membrane.
- Mechanisms:
- Lack of target structure (没有靶点结构).
- Impermeable to the antibiotic (对药物不通透).
2. Acquired Resistance (获得性耐药)
A previously sensitive organism becomes resistant.
- Driver: Darwinian Evolution / Natural Selection (自然选择).
- In a large population of bacteria (e.g., $10^8$ cells), a rare mutation may occur.
- Applying an antibiotic kills the susceptible population (Susceptible cells).
- The resistant mutant survives and proliferates (Selection pressure).
3. Mechanisms of Resistance (耐药机制) - How the drug fails
There are four main molecular mechanisms by which bacteria resist drugs:
A. Enzymatic Inactivation (酶活灭活)
The bacteria produce enzymes that destroy or modify the drug.
- Example: Beta-lactamases ($\beta$-内酰胺酶) hydrolyse the beta-lactam ring of penicillins and cephalosporins.
- Counter-strategy: Use Beta-lactamase inhibitors (e.g., Clavulanic acid).
B. Modification of the Target (靶点修饰)
The bacteria alter the binding site so the drug can no longer attach.
- Example: Altered PBP (Penicillin Binding Protein) in MRSA (Methicillin-Resistant S. aureus).
- Example: Methylation of the ribosome prevents macrolide binding.
C. Reduced Permeability / Downregulation of Porins (降低通透性)
The bacteria stop the drug from entering the cell.
- Common in Gram-negative bacteria (e.g., Pseudomonas aeruginosa).
- They close or downregulate Porin channels (孔蛋白通道) in the outer membrane.
D. Efflux Pumps (外排泵)
The bacteria actively pump the drug out of the cell before it can reach a toxic concentration.
- These are transmembrane proteins that eject antibiotics.
E. Biofilms (生物膜) - A Physiological Mechanism
- Definition: An aggregate of microorganisms in which cells adhere to each other and/or to a surface.
- Examples: Dental plaque (牙菌斑), infections on catheters, heart valves, hip replacements.
- Resistance: Biofilms are phenotypically resistant (表型耐药), not necessarily genetically resistant.
- They require up to 1000x higher concentration of antimicrobial to kill compared to planktonic (floating) bacteria.
- Mechanism: Slow growth rate, physical barrier matrix, altered microenvironment.
4. Transmission of Resistance (耐药性的传播) - How genes move
Bacteria can acquire resistance genes via Horizontal Gene Transfer (HGT/水平基因转移).
- Transformation (转化):
- Uptake of “naked” extracellular DNA from the environment (often from dead bacteria) into the cell.
- Conjugation (接合):
- “Bacterial Mating”. Transfer of DNA (usually Plasmids) via direct cell-to-cell contact using a Pilus (菌毛).
- This is a major route for the spread of multi-drug resistance plasmids in hospitals.
- Transduction (转导):
- Transfer of DNA via Bacteriophages (噬菌体) (viruses that infect bacteria). The virus accidentally packages bacterial DNA and injects it into a new host.
5. Drivers of Resistance (耐药性的驱动因素)
- Overuse and Misuse (过度使用和滥用): Prescribing antibiotics for viral infections (colds, flu).
- Agricultural Use (农业用途):
- Using antibiotics as growth promoters (Prophylactic use in livestock).
- Risk: Resistant bacteria from animals enter the human food chain (Trophallaxis concept).
- Inadequate Infection Control: Poor hygiene in hospitals allows resistant clones to spread.
- Global Travel: Resistance mechanisms (e.g., NDM-1) spread rapidly across continents.
- Lack of New Drugs: The “Discovery Void”. Developing new antibiotics is expensive (~£1 billion) and difficult, leading to a lack of new drug classes since the 1980s.
The “One Health” Concept (全健康/同一健康理念)
Recognizing that human health, animal health, and the environment are interconnected. Antibiotics released into the environment (sewage, manure) affect resistance in humans.
6. Clinical Consequences & Specific Pathogens
Key Resistant Organisms
- MRSA: Methicillin-Resistant Staphylococcus aureus.
- VRE: Vancomycin-Resistant Enterococci.
- ESBL: Extended-Spectrum Beta-Lactamase producing bacteria (break down cephalosporins).
- CRE: Carbapenem-Resistant Enterobacteriaceae (Resistance to “last-resort” drugs).
Consequences
- Treatment failure.
- Increased mortality and morbidity.
- Prolonged hospital stays.
- Increased healthcare costs.
7. Antimicrobial Stewardship (抗微生物药物管理/导向)
Definition: An organisational or healthcare-system-wide approach to promoting and monitoring judicious use of antimicrobials to preserve their future effectiveness.
Key Strategies (AMS Strategies)
- Diagnosis & Guidelines:
- Only prescribe when there is clinical evidence of bacterial infection.
- Follow local formulary/guidelines (First-line vs Second-line drugs).
- Start Smart, Then Focus (精明开始,然后聚焦):
- Start Smart: If a patient is critically ill (e.g., Sepsis), start broad-spectrum antibiotics immediately (within 1 hour) after taking cultures.
- Then Focus (The 48-Hour Review): Review the prescription at 48-72 hours.
- Options:
- Stop: If no infection is found.
- Switch: IV to Oral (if patient improves).
- Change: To a narrower spectrum agent based on culture results (De-escalation).
- Continue: If indicated.
- OPAT: Outpatient Parenteral Antibiotic Therapy.
- Options:
- Surgical Prophylaxis (外科预防):
- Single dose given <60 minutes before incision.
- Do not continue for days after surgery (unless infection is present).
- Combination Therapy:
- Using multiple drugs to reduce the statistical probability of resistance developing (e.g., in Tuberculosis treatment).
Summary for Pharmacists
- Understand the mechanism of action vs mechanism of resistance.
- Promote compliance (completing courses).
- Challenge unnecessary prescriptions.
- Understand One Health and the global nature of the problem.
LECTURE8 01 Core Concept 6 Vaccination
Lecturer: Andrew McBain
Topic: Principles of Vaccination, Immune Response, and UK Schedules
1. Public Health (公共卫生)
Definition: The prevention and management of diseases and other health conditions through surveillance and promotion of healthy behaviours, communities, and environments.
Key Contributors to Health
While infectious diseases (like HIV) or accidents are visible causes of death, many major causes of morbidity (发病率) and mortality (死亡率) are preventable through lifestyle changes (diet, smoking).
Public Health Measures
Interventions that reduce disease burden include:
- Sanitation (卫生设施): Sewage treatment.
- Hand washing: Crucial in hospitals to prevent infection spread.
- Barrier contraception: Prevents sexually transmitted infections (STIs).
- Vaccination (疫苗接种): A major tool for disease prevention.
- Antibiotic Stewardship: Appropriate use of antibiotics.
- Needle exchange schemes: Reduces blood-borne viruses.
2. Dynamics of Infectious Disease (传染病动态)
Stages of Infection
When a person is infected, they progress through specific stages (which may overlap):
- Infection Point: Entry of the pathogen.
- Incubation Period (潜伏期): Time between infection and symptom onset.
- Latent Period (隐伏期): Time when the person is infected but not yet infectious (e.g., HIV can be latent for years).
- Clinical Disease: Symptoms are apparent.
- Period of Communicability (传染期): The window during which the host can infect others. Note: This can occur before symptoms appear or after recovery.
The Chain of Infection (感染链)
Transmission relies on a chain. Vaccination breaks the link of the Susceptible Host (易感宿主).
- Germs/Agent: Bacteria, Viruses, Parasites.
- Reservoir: Where germs live (people, animals, food, soil).
- Portal of Exit: How germs leave (vomit, saliva, blood, stool).
- Mode of Transmission: Contact, droplets.
- Portal of Entry: Mouth, cuts, eyes.
- Susceptible Host: Babies, elderly, unimmunised people.
3. Immunity: Innate vs Adaptive (免疫:先天性与适应性)
Innate Immunity (先天性免疫)
- Definition: Non-inducible ability to recognise and destroy pathogens. Does not require previous exposure.
- Characteristics: No memory, non-specific.
- Physical/Chemical Barriers:
- Lysozyme (溶菌酶): In tears/secretions, dissolves bacterial cell walls.
- Normal Microbiota (正常菌群): Compete with pathogens for space/nutrients (Skin, Gut).
- Skin: Physical barrier, fatty acids.
- Stomach Acidity: pH 2 kills most microbes.
- Mucociliary Escalator (黏液纤毛阶梯): Mucus traps microbes; cilia move them out (impaired in smokers).
- Flushing action: Urine flow, blinking (tears).
- Cellular Component: Phagocytes (吞噬细胞) (e.g., Neutrophils, Macrophages) recognise common Pathogen-Associated Molecular Patterns (PAMPs) via Pattern Recognition Receptors (PRRs) and engulf them.
Adaptive Immunity (适应性免疫)
- Definition: The acquired ability (获得性能力) to recognise and destroy a specific pathogen.
- Characteristics: Specificity (recognises antigens), Memory (记忆), Tolerance (does not attack self).
- Mechanism:
- Relies on B-cells and T-cells.
- Upon exposure to an antigen (Ag), B-cells undergo Clonal Expansion (克隆扩增).
- Differentiate into Plasma Cells (secrete antibodies) and Memory Cells.
- Immunological Memory:
- Primary Response: Slow (days/weeks), weak.
- Secondary Response: Rapid, robust (stronger), specific. This is the biological basis of vaccination.
Antibodies (Immunoglobulins) (抗体/免疫球蛋白)
- IgM & IgG: Found in blood/tissue fluids. Main systemic defence.
- IgA: Found in Secretions (分泌物) (mucus, tears, breast milk, gut). Protects mucosal surfaces.
- IgE: Involved in allergy and parasite defence.
- IgD: B-cell receptor.
Functions: Antibodies bind pathogens (Neutralisation), coat them for phagocytosis (Opsonisation), or activate Complement.
4. Types of Acquired Immunity (获得性免疫的类型)
| Type | Active (Immune system actively produces antibodies) | Passive (Antibodies received externally) |
|---|---|---|
| Natural (自然) | Infection: Recovery from disease. | Maternal: Placental transfer (IgG) or Breast milk (IgA). Protects neonates temporarily. |
| Artificial (人工) | Vaccination: Exposure to harmless antigen to induce memory. | Antiserum/Immunoglobulin Injection: Injection of pre-formed antibodies (e.g., Snake anti-venom, Tetanus immunoglobulin). Immediate but short-lived protection. |
5. Vaccine Strategies (疫苗策略)
The goal is to induce active immunity (memory) without causing disease.
Main Types
- Live Attenuated (减毒活疫苗): Pathogen is viable but weakened (virulence reduced).
- Examples: MMR, Sabin Polio (Oral), BCG, Rotavirus, Shingles (Zostavax).
- Inactivated / Killed (灭活/死疫苗): Pathogen is killed (heat/chemicals).
- Examples: Salk Polio (Injection), Pertussis, Flu (most types).
- Subunit / Toxoid (亚单位/类毒素): Only parts of the pathogen or inactivated toxin.
- Examples: Tetanus toxoid, Diphtheria toxoid, Hib, MenB, HPV (Virus-like particle), Hepatitis B.
- Newer Technologies: mRNA (COVID-19), Viral Vector.
Comparison: Live vs Inactivated (重要对比)
| Feature | Live Attenuated (e.g., Sabin Polio) | Inactivated (e.g., Salk Polio) |
|---|---|---|
| Immune Response | Stronger, mimics natural infection. Induces IgA (Mucosal immunity) and IgG. | Weaker. Induces mainly IgG (Systemic immunity). Little/No IgA. |
| Doses | Fewer doses (often single). Replicates in host. | Multiple doses/boosters required. |
| Adjuvant (佐剂) | Not usually required. | Required (e.g., Aluminium salts) to boost response. |
| Stability | Unstable. Requires Cold Chain (冷链). | More stable. |
| Safety Risk | Risk of Reversion (返祖) to virulence (rare). Can infect others. Avoid in immunocompromised. | Safe. Cannot revert or cause disease. |
Case Study: Polio Vaccines (脊髓灰质炎疫苗)
- Sabin (Oral Polio Vaccine - OPV): Live. Induces gut immunity (IgA). Prevents the virus replicating in the gut, stopping transmission. Risk: Vaccine-derived polio.
- Salk (Inactivated Polio Vaccine - IPV): Killed (injected). Induces blood immunity (IgG). Prevents the virus reaching the nerves (paralysis), but does not prevent gut infection/transmission.
- Current UK Strategy: Uses IPV (Salk) to eliminate the risk of vaccine-derived polio, as wild polio is eliminated in the UK.
6. UK Vaccination Schedule (UK 免疫计划)
Note: Schedules change; this is based on the general principles discussed.
Key Principles
- Timing (8, 12, 16 weeks): Vaccination starts at 2 months. It is not done at birth (except Hep B for risk groups/BCG) because Maternal Antibodies (母体抗体) may interfere with the vaccine and the infant’s immune system is still developing.
- Herd Immunity (群体免疫): High vaccination coverage (~80-95%) protects the unvaccinated (e.g., immunocompromised) by breaking the chain of transmission.
Specific Vaccines Mentioned
- 6-in-1 Vaccine (Hexavalent): Diphtheria, Tetanus, Pertussis (Whooping cough), Polio (IPV), Hib, Hepatitis B. Given at 8, 12, 16 weeks.
- Rotavirus: Oral vaccine for gastroenteritis.
- Meningitis Vaccines (MenB, MenC, MenACWY): Meningitis is a medical emergency (can kill/disable). High priority.
- MMR: Measles (麻疹), Mumps (流行性腮腺炎), Rubella (风疹).
- Rubella importance: Prevents Congenital Rubella Syndrome (birth defects) if a pregnant woman is infected.
- Controversy: The Wakefield paper falsely linked MMR to autism, causing a drop in uptake and outbreaks of measles.
- HPV (Human Papillomavirus):
- Target: Prevents Cervical cancer (females) and Head/Neck cancers (males). Also prevents genital warts.
- Given to adolescents (boys and girls now).
- Shingles (带状疱疹): Reactivation of chickenpox virus. Vaccine for older adults (70s).
LECTURE10 01 Core Concept 8 GI Pharmacology & Therapeutics H pylori and C difficile
Lecturer: Sarah Knighton
Part 1: Helicobacter pylori (H. pylori)
1. Overview & Pathophysiology
-
Organism: Gram-negative bacteria (革兰氏阴性菌).
-
Infection Site: Persistently infects the gastroduodenal mucosa (胃十二指肠黏膜).
-
Consequences: Infection always causes gastritis (胃炎), which can be acute or chronic.
-
Peptic Ulcer Disease (PUD, 消化性溃疡): H. pylori is the most common cause.
- ~95% of Duodenal Ulcers (十二指肠溃疡).
- ~70-80% of Gastric Ulcers (胃溃疡).
-
Malignancy Risk: Linked to gastric cancer and MALT lymphoma (黏膜相关淋巴组织淋巴瘤).
-
Transmission: Unclear, likely gastro-oral or faeco-oral.
-
Prevalence: Increases with age; approx. 50% of the global population is infected (often asymptomatic).
2. Clinical Presentation of PUD
Symptoms can be non-specific (heartburn, bloating, nausea). Key features of ulcer pain:
- Well-localised (patients can point to specific spot).
- Nature: Sharp, stabbing, gnawing pain in the midepigastrium (上腹部).
Symptom Comparison (Important for Diagnosis)
| Feature | Gastric Ulcer (胃溃疡) | Duodenal Ulcer (十二指肠溃疡) |
|---|---|---|
| Pain Timing | When stomach is empty. | 2-3 hours after eating (post-prandial). |
| Effect of Food | Relieved by food (Food acts as a buffer). | Worsens 2-3 hours later (Acid/food moves to duodenum). |
| Night Pain | Less common. | Can be worse at night-time. |
Note: Host co-factors (e.g., NSAID use) are also critical in ulcer development.
Red Flags (ALARM Symptoms)
If these are present, urgent referral/investigation is needed to rule out cancer or severe bleeding.
- A - Anaemia (贫血) (tiredness, SOB).
- L - Loss of weight (unintentional).
- A - Anorexia (厌食) (unexplained appetite loss).
- R - Recent onset of progressive symptoms.
- M - Melaena (黑便) / Haematemesis (呕血).
- S - Swallowing problems (Dysphagia, 吞咽困难).
3. Diagnosis
Confirmation is required before starting eradication therapy.
Diagnostic Methods
-
Urea Breath Test (UBT, 尿素呼气试验): Standard non-invasive test.
-
Patient swallows $^{13}$C-labelled urea.
-
If H. pylori is present, its urease (脲酶) breaks urea down into labelled CO$_2$.
-
Labelled CO$_2$ is detected in breath.
-
-
Stool Antigen Test (SAT).
-
Endoscopy (Gastroscopy):
-
CLO Test (Rapid Urease Test): Biopsy placed in urea solution; colour change indicates pH rise due to ammonia production.
-
Histology/Culture.
-
Crucial Drug Interactions with Testing (False Negatives)
Medications can suppress bacteria or urease activity, leading to false negative results.
graph TD
A[Patient needs H. pylori Test] --> B{Is patient on meds?}
B – Yes: Antibiotics --> C[Stop 4 weeks before test]
B – Yes: PPIs (e.g., Omeprazole) --> D[Stop 2 weeks before test]
B – No --> E[Proceed with Test]
C --> E
D --> E
4. Management: Eradication Therapy (根除治疗)
Standard Regimen: Triple Therapy (3 drugs) for 7 Days, taken Twice Daily (BD).
- Components: 1 PPI + 2 Antibiotics.
- Adherence: Critical for success.
First Line Treatment Algorithms
| Patient Status | Regimen (All doses BD for 7 days) | Notes |
|---|---|---|
| No Penicillin Allergy | PPI (Full Dose) + Amoxicillin (1g) + Clarithromycin (500mg) OR Metronidazole (400mg) | Choose Clarithromycin or Metronidazole based on interactions/history. |
| Penicillin Allergy | PPI (Full Dose) + Clarithromycin (500mg) + Metronidazole (400mg) | Avoid Amoxicillin. |
- Full Dose PPI examples: Lansoprazole 30mg, Omeprazole 20-40mg.
Key Drug Interactions (Pharmacist’s Role)
-
Clarithromycin + Statins (e.g., Atorvastatin/Simvastatin):
-
Risk: Myopathy/Rhabdomyolysis (Clarithromycin inhibits CYP3A4, increasing statin levels).
-
Management: Stop the statin during the 7-day antibiotic course.
-
-
Metronidazole + Alcohol:
-
Risk: Disulfiram-like reaction (flushing, vomiting).
-
Management: Avoid alcohol during treatment and for 48 hours after.
-
Post-Treatment
- Retesting: Not routine if symptoms resolve.
- Indications to retest: Persistent/recurrent symptoms, or complicated ulcer. (Must use UBT, wait 6-8 weeks after treatment).
Part 2: Clostridioides difficile (C. diff)
1. Overview
-
Organism: Gram-positive, spore-forming, anaerobic rod.
-
Pathology: Often an asymptomatic commensal (2-3% of adults).
-
Antibiotics suppress normal gut flora $\rightarrow$ C. diff overgrows $\rightarrow$ Produces toxins.
- Toxins cause inflammation, mucosal damage, and diarrhoea.
-
Severity: Mild diarrhoea $\rightarrow$ Pseudomembranous colitis (伪膜性结肠炎) $\rightarrow$ Bowel perforation $\rightarrow$ Death.
2. Risk Factors
-
Antibiotics (The “4 C’s” are high risk):
- Clindamycin
- Cephalosporins (e.g., Ceftriaxone)
- Ciprofloxacin (Fluoroquinolones)
- Co-amoxiclav (Broad-spectrum penicillins)
-
Medications: PPIs (Acid suppression alters gut environment).
-
Patient Factors: Age > 65, prolonged hospitalisation, underlying morbidity.
3. Diagnosis & Management
- Symptoms: Unexplained diarrhoea (distinctive smell), abdominal pain, fever, raised WBC (leukocytosis).
- Diagnosis: Stool test for C. diff Toxin.
Immediate Management Protocol (SIGHT Mnemonic)
- S - Suspect (if unclear cause of diarrhoea).
- I - Isolate patient (within 2 hours).
- G - Gloves and aprons (PPE).
- H - Hand washing with soap and water. (Alcohol gel does NOT kill spores).
- T - Test stool immediately.
Pharmacological Management
-
Stop Offending Agents:
-
Stop the causative antibiotic (if clinical condition allows).
-
Stop PPIs.
-
STOP Anti-motility drugs (e.g., Loperamide): These prevent toxin clearance and can cause toxic megacolon.
-
-
Specific Treatment (NICE Guidelines):
-
First Line: Vancomycin (Oral) 125mg QDS for 10 days.
- Note: Must be oral (IV Vancomycin does not penetrate the gut lumen effectively).
-
Second Line: Fidaxomicin (Oral).
-
Severe/Life-threatening: Oral Vancomycin + IV Metronidazole.
-
-
Recurrent/Refractory:
-
Faecal Microbiota Transplant (FMT, 粪菌移植): Restore healthy gut flora.
-
IV Immunoglobulin.
-
Summary Checklist for Revision
- [ ] Understand the Triple Therapy regimen for H. pylori (Doses/Duration).
- [ ] Know the washout periods for PPIs (2 weeks) and Antibiotics (4 weeks) before H. pylori testing.
- [ ] Identify the interaction between Clarithromycin and Statins.
- [ ] Recognize the “4 C’s” antibiotics that trigger C. diff.
- [ ] Remember to stop Loperamide in C. diff infection.
LECTURE14 01 Core Concept 12 Immune-mediated inflammatory disease - IBD therapeutics
1. Introduction & Epidemiology (简介与流行病学)
- Prevalence: Affects ~1 in 250 people in the UK. Increasing incidence globally.
- Peak Onset: 15–30 years old (early adulthood).
- Etiology (病因): A complex interaction of Genetics, Environment, and Dysregulated Immune Response to intestinal microbiota.
Risk Factors & Environmental Triggers
| Factor | Crohn’s Disease (CD) | Ulcerative Colitis (UC) |
|---|---|---|
| Smoking | Aggravates disease (Risk factor) | Protective (Smoking cessation can trigger onset) |
| Appendectomy | Increased risk (slightly) | Protective (Reduced risk) |
| Genetics | High concordance (NOD2/CARD15 gene) | Moderate concordance |
| Diet/Stress | Triggers exacerbations | Triggers exacerbations |
2. Comparison: Crohn’s vs. Ulcerative Colitis (核心区别)
| Feature | Ulcerative Colitis (UC) | Crohn’s Disease (CD) |
|---|---|---|
| Location | Colon only (Starts rectum, extends proximally) | Anywhere (Mouth to Anus). Terminal ileum is most common. |
| Distribution | Continuous inflammation (连续性) | Skip lesions (跳跃性病变 - patchy) |
| Depth | Mucosal (Superficial - 粘膜层) | Transmural (Full thickness - 全层) |
| Histology | Crypt abscesses, goblet cell depletion | Granulomas (肉芽肿), deep fissures |
| Symptoms | Bloody diarrhoea, urgency, tenesmus | Abdominal pain, weight loss, non-bloody diarrhoea |
| Complications | Toxic megacolon, Cancer risk | Fistulas (瘘管), Strictures (狭窄), Abscesses |
3. Pathophysiology (病理生理)
- Mechanism: Loss of tolerance to gut bacteria $\rightarrow$ Chronic inflammation.
- Key Cytokines:
- TNF-$\alpha$: Central driver of inflammation in both.
- Interleukins: IL-12, IL-23, IL-17, IL-6.
- Integrins ($\alpha_4\beta_7$): Direct leukocytes into the gut tissue.
4. Diagnostics (诊断)
- Stool Test: Faecal Calprotectin (Biomarker of neutrophil intestinal inflammation). Helps distinguish IBD from IBS.
- Endoscopy: Colonoscopy with biopsy is the Gold Standard.
- Imaging: MRI/CT (to check for small bowel disease in CD).
5. Pharmacology: Drug Classes (药物类别)
A. Aminosalicylates (5-ASAs)
- Drugs: Mesalazine (Oral/Rectal), Sulfasalazine, Olsalazine.
- MOA: Unclear, likely PPAR-$\gamma$ agonist, inhibits NF-$\kappa$B, reduces cytokine production. Topically active on the gut mucosa.
- Formulations: pH-dependent coatings (e.g., Asacol, Pentasa) allow drug release in the colon/ileum to avoid stomach absorption.
- Clinical Use:
- First-line for Mild-Moderate UC (Induction & Maintenance).
- Less effective in Crohn’s Disease.
B. Corticosteroids (皮质类固醇)
- Drugs: Prednisolone (Oral/IV), Hydrocortisone (IV), Budesonide (Oral/Rectal).
- MOA: Broad anti-inflammatory.
- Budesonide: High first-pass metabolism $\rightarrow$ Low systemic bioavailability $\rightarrow$ Fewer side effects. Used for mild-moderate Ileal Crohn’s.
- Clinical Use:
- Induction of Remission ONLY (Acute Flares).
- NOT for Maintenance (Due to long-term toxicity: osteoporosis, diabetes, Cushing’s).
C. Thiopurines (Immunomodulators)
- Drugs: Azathioprine (AZA), Mercaptopurine (6-MP).
- MOA: Purine antimetabolites $\rightarrow$ Inhibit DNA/RNA synthesis in T/B cells $\rightarrow$ Induce T-cell apoptosis.
- Clinical Use:
- Maintenance Therapy (Steroid-sparing agents).
- Onset of action is slow (3–6 months).
- Safety:
- TPMT Test: Must check Thiopurine Methyltransferase (TPMT) levels before starting. Low levels $\rightarrow$ High toxicity (Bone marrow suppression).
- Monitor FBC and LFTs regularly.
D. Methotrexate (MTX)
- MOA: Folic acid antagonist.
- Clinical Use: Maintenance in Crohn’s Disease (if AZA fails/intolerant). Generally not used for UC.
- Safety: Teratogenic (Must use contraception), Hepatotoxic.
E. Biologics (Biological Therapies - Monoclonal Antibodies)
Used for Moderate-Severe disease refractory to conventional therapy.
-
Anti-TNF Agents:
- Infliximab (IV), Adalimumab (SC).
- Use: Induction & Maintenance for both UC and CD.
- Risk: Reactivation of TB/Hepatitis B. Must screen before starting.
- Issue: Immunogenicity (Body creates Anti-Drug Antibodies $\rightarrow$ Loss of response).
-
Anti-Integrin Agents (Gut-Selective):
- Vedolizumab.
- MOA: Blocks $\alpha_4\beta_7$ integrin on lymphocytes, preventing them from entering the gut tissue.
- Advantage: Gut-specific, less systemic immunosuppression.
-
Anti-IL-12/23 Agents:
- Ustekinumab.
- Use: Particularly effective in Crohn’s Disease.
F. JAK Inhibitors (Small Molecules)
- Drugs: Tofacitinib, Filgotinib, Upadacitinib.
- MOA: Oral Janus Kinase inhibitors. Block intracellular signaling pathways for cytokines.
- Use: Moderate-Severe Ulcerative Colitis.
- Pros: Oral administration (Tablets), rapid onset (unlike Thiopurines).
- Risks: VTE (Clots), Herpes Zoster (Shingles).
6. Management Strategies (治疗策略)
Ulcerative Colitis Management
- Mild-Moderate (Proctitis/Left-sided):
- 1st Line: Topical 5-ASA (Suppository/Enema).
- 2nd Line: Oral 5-ASA + Topical 5-ASA.
- Moderate-Severe (Extensive):
- Oral Steroids (Prednisolone) for induction.
- Maintenance: Thiopurines or Biologics (Anti-TNF, Vedolizumab) or JAK inhibitors.
- Acute Severe UC (Medical Emergency):
- Criteria: $\ge$ 6 bloody stools/day + systemic toxicity (HR>90, Temp>37.8, CRP>45).
- Rx: Hospitalisation, IV Hydrocortisone.
- Rescue Therapy (Day 3 if no response): Infliximab or Ciclosporin.
Crohn’s Disease Management
- Induction:
- Steroids: Prednisolone or Budesonide.
- EEN (Exclusive Enteral Nutrition): Liquid diet only for 6-8 weeks. First-line induction for children (avoids steroid growth suppression).
- Maintenance:
- Azathioprine / Mercaptopurine.
- Methotrexate.
- Biologics: Infliximab, Adalimumab, Ustekinumab.
- Surgery: Not curative (disease can recur at anastomosis site), but used for complications (strictures/fistulas).
7. Pharmacist’s Role & Counselling (药师角色)
- Smoking: Strong advice to stop for Crohn’s patients.
- Blood Monitoring: Crucial for Azathioprine (Bone marrow) and Methotrexate (Liver).
- Vaccines:
- Patients on Biologics/High-dose steroids are immunocompromised.
- NO Live Vaccines (e.g., Yellow Fever, MMR).
- Annual Flu jab and Pneumococcal vaccine recommended.
- Cancer Risk: Long-term colitis increases colorectal cancer risk $\rightarrow$ Need surveillance colonoscopies. Long-term Thiopurines slightly increase skin cancer/lymphoma risk.
LECTURE17 01 Core Concept 15 Skin therapeutics
Lecturer: Mary Rhodes
1. Skin Structure & Function
Chinese Term: 皮肤结构与功能
A. Structure
The skin is the largest organ (16% of body weight). Key layers involved in these diseases:
- Epidermis (表皮):
- Keratinocytes (角质形成细胞): The main cell type. They move from the basal layer to the top, flattening and dying to form the barrier (Stratum corneum).
- Relevance: Psoriasis involves hyperproliferation of these cells.
- Dermis (真皮): Contains blood vessels, nerve endings, sweat glands, sebaceous glands.
- Hypodermis (皮下组织): Subcutaneous fat.
B. Key Functions
- Barrier: Protects against bacteria, toxins, dehydration, UV radiation.
- Sensory: Touch, pain, pressure, temperature, itch (pruritus).
- Thermoregulation: Vasodilation/vasoconstriction, sweating.
- Synthesis: Vitamin D production.
- Immune Response: Langerhans cells detect pathogens $\rightarrow$ T-cell activation.
2. Atopic Eczema (Dermatitis)
Chinese Term: 特应性湿疹 (皮炎)
A. Epidemiology & Risk Factors
- Atopic Triad: Strong link with Asthma and Hay fever (Allergic Rhinitis).
- Onset: Usually in childhood (< 5 years); can persist or recur in adulthood.
- Triggers:
- External: Soap, detergents, wool, pollen, dust mites, extreme temperatures (cold/heat).
- Internal: Stress, hormones, genetics, food allergies (rarely).
B. Pathophysiology (病理生理)
- Barrier Defect: Altered keratinocyte differentiation (filaggrin defect) $\rightarrow$ Water loss (Dryness).
- Immune Dysregulation: T-helper cell activation $\rightarrow$ Inflammation.
- Result: Dysfunctional barrier + Hyper-reactivity to irritants.
C. Clinical Features
- Symptoms: Intense Itch (Pruritus), dry skin, inflammation.
- Distribution (Location):
- Typically affects Flexures (insides of elbows, backs of knees - 屈侧).
- Face, neck, and hands are also common.
- Appearance: Erythema (redness), papules (丘疹), plaques (斑块). Can become weeping/crusted if infected (S. aureus).
D. Management Strategy
Goal: Restore barrier + Reduce inflammation.
1. Emollients (润肤剂) - Mainstay of treatment
- Role: Restore skin integrity, prevent water loss, steroid-sparing effect.
- Usage:
- Apply frequently and liberally (4-5 times/day).
- Use even when skin is clear.
- Apply in direction of hair growth (to avoid folliculitis).
- Safety: Paraffin-based products are flammable (fire risk with smoking).
- Formulations:
- Ointments (软膏): Greasy, no preservatives (less irritation), best for very dry skin.
- Creams (乳膏): Lighter, absorb quickly, contain preservatives (may sting).
- Lotions/Gels: Lightest.
- Avoid: Aqueous Cream (contains Sodium Lauryl Sulphate - irritant).
2. Topical Corticosteroids (局部皮质类固醇) - For Flare-ups
-
Role: Anti-inflammatory for active flares.
-
Usage: Apply sparingly, usually OD or BD, max 4 weeks.
-
Dosing Unit: Finger Tip Unit (FTU, 指尖单位).
- 1 FTU = line of cream from distal crease to tip of index finger (~0.5g).
- 1 FTU covers an area of 2 flat hands.
-
Potency Hierarchy (Important for prescribing):
Potency Example Chinese Mild Hydrocortisone 0.1% - 2.5% 弱效 (氢化可的松) Moderate Clobetasone butyrate (Eumovate) 中效 Potent Betamethasone valerate (Betnovate) 强效 Very Potent Clobetasol propionate (Dermovate) 超强效 (Specialist only) -
Side Effects: Skin atrophy (thinning), striae (stretch marks), telangiectasia (thread veins), rebound flare upon stopping.
3. Second-Line & Adjuncts
- Topical Calcineurin Inhibitors (e.g., Tacrolimus, Pimecrolimus):
- Use: If steroids are ineffective or unacceptable risk (e.g., on face/neck).
- Antihistamines:
- Sedating (e.g., Chlorphenamine): If itch disturbs sleep (short term 7-14 days).
- Non-sedating: Generally not recommended unless urticaria is present.
- Bandages/Wet Wraps: For severe cases (Specialist).
3. Psoriasis (Chronic Plaque)
Chinese Term: 银屑病 (寻常型)
A. Pathophysiology
- Hyperproliferation: Keratinocytes grow too fast (turnover days instead of weeks).
- Inflammation: T-cell mediated autoimmune response.
- Vascular changes: Dilated capillaries (leads to redness/bleeding).
B. Clinical Features
- Symptoms: Well-defined red plaques with silvery/white scales (银白色鳞屑). Less itchy than eczema.
- Distribution:
- Typically affects Extensors (outside of elbows, knees - 伸侧).
- Scalp, lower back, buttocks.
- Nail Changes: Pitting (点状凹陷), onycholysis (separation from nail bed).
- Complications:
- Psoriatic Arthritis (银屑病关节炎): Joint pain.
- Metabolic Syndrome: Increased risk of CVD (Cardiovascular Disease), obesity, diabetes.
- Mental Health: Depression/Anxiety.
C. Management Strategy
1. Topical Therapies (First Line)
- Emollients: Reduce scaling and dryness.
- Vitamin D Analogues (e.g., Calcipotriol):
- Mechanism: Inhibits keratinocyte proliferation.
- Note: Often combined with steroids (e.g., Dovobet).
- Coal Tar (煤焦油): Anti-inflammatory and anti-scaling. Smells and stains.
- Dithranol: Effective but stains skin purple/brown. Used for difficult plaques.
- Topical Steroids: For flares, usually combined with Vit D or coal tar.
2. Phototherapy (光疗)
- UVB or PUVA (Psoralen + UVA).
3. Systemic/Biologic Therapy (Severe Cases - Specialist)
- Methotrexate, Ciclosporin, Acitretin.
- Biologics (e.g., Adalimumab, Secukinumab).
Comparison: Eczema vs. Psoriasis
| Feature | Eczema (湿疹) | Psoriasis (银屑病) |
|---|---|---|
| Site | Flexures (inside elbow/knee) | Extensors (outside elbow/knee) |
| Itch | Intense (Define feature) | Mild or absent |
| Appearance | Indistinct borders, dry, weeping | Well-defined plaques, silvery scales |
| Pathology | Barrier defect + Allergy | Hyperproliferation |
4. Acne Vulgaris
Chinese Term: 寻常痤疮
A. Pathophysiology
- Hormones: Androgens increase Sebum (oil) production.
- Hyperkeratinisation: Dead skin cells block the follicle (Comedonegenesis).
- Bacteria: Colonisation by Cutibacterium acnes (C. acnes).
- Inflammation: Pus formation.
B. Clinical Features
- Comedones (粉刺): Blackheads (open) and Whiteheads (closed).
- Inflammatory: Papules, Pustules (pus-filled).
- Severe: Nodules, Cysts (risk of scarring).
- Sites: Face, back, chest (seborrhoeic areas).
C. Management Strategy
Take time to work (up to 8 weeks for improvement).
Lifestyle Advice:
- Do not over-clean (irritates skin).
- Do not squeeze/pick (scarring risk).
- Use non-comedogenic products.
Pharmacological Step-Up:
| Severity | Treatment Options | Chinese Notes |
|---|---|---|
| Mild to Moderate | Topical Retinoids (Adapalene) + Benzoyl Peroxide (BPO) | 维A酸类 + 过氧化苯甲酰 BPO会导致头发/衣物漂白 (Bleaching) |
| Moderate | Topical Antibiotic (Clindamycin) + BPO / Retinoid (Do not use monotherapy antibiotic due to resistance) | 局部抗生素 必须联合使用以防耐药 |
| Moderate (Widespread) | Oral Antibiotics (Lymecycline/Doxycycline) + Topical BPO/Retinoid (Max 3 months usually) | 口服抗生素 (四环素类) 注意光敏性 (Photosensitivity) |
| Severe | Oral Isotretinoin (Roaccutane) Specialist Prescribing Only | 异维A酸 有极强致畸性 (Teratogenic) - 必须避孕 |
Women: Combined Oral Contraceptives (COC) can help (Dianette).
5. Differential Diagnosis (Crucial for Diagnosis)
Chinese Term: 鉴别诊断
You must distinguish inflammatory conditions from infections:
- Fungal Infection (Ringworm/Tinea):
- Signs: Asymmetrical, defined active edge (ring shape), central clearing. Itchy but often shiny/macerated if in folds.
- Contact Dermatitis:
- Signs: Localised to contact site (e.g., watch strap, belt buckle, nickel allergy).
- Scabies (疥疮):
- Signs: Intense itch (worse at night), burrows (fingers, wrists, genitals). Contagious.
- Shingles (带状疱疹):
- Signs: Dermatomal distribution (stops at midline), painful vesicles/blisters, malaise.
- Rosacea (酒渣鼻):
- Signs: Facial redness/flushing, papules but NO comedones (unlike acne).
LECTURE20 01 Core Concept 17 Childhood viral disease
Lecturer: Gavin Humphreys
1. General Principles (基本原则)
- Pathogens (病原体): Viruses are genetic material (DNA or RNA) encapsulated in protein.
- Vulnerability (易感性): Children are highly susceptible due to developing immune systems and behavioural factors (poor hygiene, close contact in nurseries).
- Transmission (传播): Most childhood viruses discussed are propagated via respiratory routes or faecal-oral transmission.
2. Chickenpox (Varicella-Zoster Virus / VZV - 水痘)
Pathogenicity & Mechanism (致病性与机制)
- Virus Type: DNA virus.
- Transmission:
- Primary Route: Respiratory (Airborne/Aerosol) - 呼吸道传播.
- Infectivity: $R_0$ (Reproductive number) is 8–10 (Highly infectious).
- Pathogenesis Pathway:
- Entry: Inhalation into the Upper Respiratory Tract (URT).
- Viraemia (病毒血症): Replicates in T-cells (T-cell viraemia).
- Skin Infection: Transports via blood to skin, causing vesicle formation.
- Latency (潜伏): Virus moves via retrograde transport to sensory nerve cell bodies (Dorsal Root Ganglion).
- Reactivation: Can reactivate later in life as Shingles (带状疱疹 / Zoster), often due to stress or immunocompromise.
Epidemiology (流行病学)
- UK Context: Endemic (constantly present). Seasonal peak in March–May.
- Prevalence: 90% of adults are immune. 75% of cases occur in <5 year olds.
- Mortality: Rare (c.20 deaths/annum in UK), but risk increases significantly with age (adults).
Clinical Features (临床特征)
- Incubation Period: 10–21 days.
- Symptoms:
- Prodromal: Acute, non-specific onset (fever, malaise).
- Rash: Characteristic fluid-filled vesicles (水疱).
- Progression: Vesicles dry to form granular scabs approx. 4 days post-onset.
- Infectious Period: From onset until all scabs are dry.
Management (Pharmacy & Clinical Focus - 治疗与管理)
- Antivirals: Aciclovir (阿昔洛韦) is generally not recommended for healthy children. It is considered for individuals >14 years or adults due to higher complication risks.
- Symptomatic Relief:
- Itch (止痒): Topical calamine lotion or Chlorphenamine (antihistamine) if >1 year old.
- Pain/Fever: Paracetamol.
- Non-Pharmacological Advice:
- Fluid intake to prevent dehydration.
- Keep nails short to prevent excoriation and secondary bacterial infection (继发性细菌感染).
- Avoid school/nursery until vesicles have crusted over.
- Risk Groups: Pregnant women, smokers, and immunocompromised individuals are at higher risk of complications like viral pneumonia.
Vaccination Strategy (疫苗策略)
- Vaccine: Live attenuated (Varilrix® or Varivax®).
- UK Schedule: Not routine. Available privately (~£150) or for specific risk groups.
- Debate: The UK avoids routine vaccination to ensure the virus circulates, providing natural “boosting” to adults to prevent Shingles, though this is scientifically controversial and likely to change.
3. Rotavirus (轮状病毒)
Pathogenicity
- Virus Type: RNA virus with a triple-layer protein capsule.
- Stability: Highly environmentally stable; can survive on surfaces for days.
- Transmission: Faecal-oral (粪-口传播). Extremely low infectious dose (approx. 10 particles).
- Mechanism of Diarrhoea:
- Replication in small intestine.
- Villous Atrophy (绒毛萎缩): Lysis of cells causes villi to collapse.
- Osmotic Imbalance: Activation of chloride channels leads to water influx into the gut.
Clinical Features
- Symptoms: Severe diarrhoea (lasting 3–8 days), vomiting, stomach cramps, mild fever.
- Red Flags (Clinical Alerts - 需紧急就医指征):
- Reduced urine output (Dehydration).
- Altered responsiveness (Lethargy).
- Tachycardia or tachypnoea.
Management
- Treatment: No specific antivirals.
- Supportive:
- Oral Rehydration Salts (ORS): Critical to manage dehydration.
- Infection Control: Strict handwashing; exclusion from school/childcare for 48 hours after the last symptom.
Vaccination
- Vaccine: Rotarix (Live-attenuated, Oral).
- Schedule: 2 doses at 8 weeks and 12 weeks of age.
- Contraindications:
- SCID (Severe Combined Immunodeficiency): Screened before administration.
- In Utero Drug Exposure: Infants whose mothers took TNF-$\alpha$ inhibitors during pregnancy should defer vaccination (live vaccine risk).
- Adverse Reaction: Intussusception (肠套叠) – rare risk (1 in 100,000) where the bowel folds in on itself.
4. Measles (麻疹 / Rubeola)
Pathogenicity & Epidemiology
- Virus Type: RNA virus.
- Transmission: Airborne/Respiratory.
- Infectivity: $R_0 = 18$ (Extremely high). Requires 95% herd immunity to halt spread.
- UK Status: Endemic transmission re-established due to vaccine hesitancy (Wakefield scandal).
Clinical Features
- Incubation: 10 days.
- Symptoms:
- Prodromal: Fever, malaise, cough.
- Rash: Erythematous, maculopapular (斑邱疹) rash appearing 3–4 days post-infection.
- Complications:
- Hospitalisation: Common in infants (<1y) and adults (>25y).
- Pneumonia: Occurs in 1/20 cases.
- SSPE (Sub-acute Sclerosing Pan-encephalitis): Rare, fatal, progressive brain inflammation occurring years after infection.
Management
- Notification: Notifiable disease (法定传染病). Pharmacists/Clinicians must inform the local Health Protection Team (HPT) immediately.
- Treatment: Supportive (fluids, paracetamol/ibuprofen).
- Isolation: Avoid susceptible individuals (pregnant, immunocompromised).
5. Mumps & Rubella (流行性腮腺炎与风疹)
Mumps (流行性腮腺炎)
- Symptoms: Swelling of the parotid glands (腮腺) (“Bull neck”), fever, headache, joint pain.
- Asymptomatic: 1 in 6 cases.
- Status: Notifiable disease.
Rubella (German Measles / 风疹)
- Symptoms: Generally mild. Low-grade fever, sore throat.
- Rash: Distinctive rough/sandpaper texture.
- Congenital Risk: Dangerous for pregnant women (Congenital Rubella Syndrome).
6. MMR Vaccination & Controversy
- Vaccine: MMRvaxPro or Priorix (Live attenuated).
- Schedule:
- Dose 1: 1 year old.
- Dose 2: 3 years and 4 months.
- Efficacy: 99% after two doses.
- The Wakefield Scandal (1998): A fraudulent paper (retracted) linked MMR to autism. This caused vaccination rates to drop to ~80% in the early 2000s, leading to the resurgence of measles.
Summary Table (复习总结表)
| Disease | Pathogen Type | Transmission | Key Symptoms | Management/Vaccine Notes |
|---|---|---|---|---|
| Chickenpox (Varicella) | DNA (VZV) | Respiratory (Primary) | Vesicular rash (水疱), fever. | Not routine in UK. Aciclovir only for severe risk/adults. |
| Rotavirus | RNA | Faecal-Oral | Severe diarrhoea, dehydration. | Red Flags: Reduced urine, lethargy. Vaccine: Oral, Live (Rotarix). |
| Measles | RNA | Airborne ($R_0=18$) | Maculopapular rash (斑邱疹), cough. | Notifiable. High hospitalisation rate. MMR Vaccine. |
| Mumps | RNA | Respiratory | Parotid gland swelling (腮腺肿大). | Notifiable. MMR Vaccine. |
| Rubella | RNA | Respiratory | Rough rash, mild fever. | Notifiable. Risk in pregnancy. MMR Vaccine. |
Core Concept - Respiratory System
LECTURE26 01 Core Concept 23 Lung Physiology and function
1. Functions of the Respiratory System (呼吸系统的功能)
- Gas Exchange (气体交换): Intake of $O_2$ for metabolism and removal of $CO_2$ (waste product).
- Regulation of Body pH (pH调节): By retaining or eliminating $CO_2$, the lungs regulate blood pH (Respiratory Acidosis/Alkalosis).
- Protection (保护): Filtering pathogens and irritants; mucociliary escalator.
- Vocalization (发声): Air moving across vocal cords.
2. Structure & Anatomy (结构与解剖)
A. The Airways (气道)
Divided into two zones:
-
Conducting Zone (传导区):
- Components: Nose, Pharynx, Larynx, Trachea, Bronchi, Bronchioles (Terminal).
- Function: Warm, humidify, and filter air. No gas exchange occurs here (Anatomical Dead Space).
- Lining: Ciliated epithelium with goblet cells (secrete mucus to trap particles).
-
Respiratory Zone (呼吸区):
- Components: Respiratory Bronchioles, Alveolar Ducts, Alveoli.
- Function: Site of gas exchange.
B. The Alveoli (肺泡)
- Huge surface area (~70 $m^2$) for diffusion.
- Type I Alveolar Cells: Flat epithelial cells; form the main structure for gas exchange (thin barrier).
- Type II Alveolar Cells: Secrete Surfactant (表面活性剂).
- Surfactant Function: Reduces surface tension of water in alveoli, preventing alveolar collapse (atelectasis) and increasing compliance.
- Alveolar Macrophages: Engulf foreign particles.
3. Mechanics of Breathing (呼吸力学)
Principle: Air moves from high pressure to low pressure.
Boyle’s Law (波义耳定律): $P_1V_1 = P_2V_2$. Pressure is inversely proportional to Volume.
A. Inspiration (吸气) - Active Process
- Muscles Contract: Diaphragm flattens (moves down), External Intercostal muscles lift ribs up and out.
- Volume Increases: Thoracic cavity expands.
- Pressure Decreases: Intrapulmonary pressure drops below atmospheric pressure (negative pressure).
- Air Flow: Air rushes IN.
B. Expiration (呼气) - Passive Process (at rest)
- Muscles Relax: Diaphragm moves up, ribs move down.
- Elastic Recoil: Lungs recoil inward.
- Volume Decreases: Thoracic cavity shrinks.
- Pressure Increases: Intrapulmonary pressure rises above atmospheric pressure.
- Air Flow: Air flows OUT.
- Forced Expiration: Uses internal intercostals and abdominal muscles (Active).
C. Intrapleural Pressure (胸膜腔内压)
- Always negative (sub-atmospheric) relative to alveolar pressure.
- This “suction” keeps the lungs inflated and attached to the chest wall.
- Pneumothorax (气胸): If air enters the pleural space, the negative pressure is lost, and the lung collapses.
4. Lung Volumes & Capacities (肺容积与容量 - Spirometry)
- Tidal Volume (TV, 潮气量): Volume of air moved during a normal breath (~500 ml).
- Inspiratory Reserve Volume (IRV, 吸气储备量): Max volume inhaled after a normal inspiration.
- Expiratory Reserve Volume (ERV, 呼气储备量): Max volume exhaled after a normal expiration.
- Residual Volume (RV, 残气量): Volume remaining in lungs after max expiration (prevents collapse). Cannot be measured by simple spirometry.
Capacities (Combinations):
- Vital Capacity (VC, 肺活量): $TV + IRV + ERV$. Total exchangeable air.
- Total Lung Capacity (TLC, 肺总量): $VC + RV$.
- Functional Residual Capacity (FRC): $ERV + RV$. Volume at the end of normal expiration.
Diagnostic Ratios (FEV1/FVC):
- FEV1: Forced Expiratory Volume in 1 second.
- FVC: Forced Vital Capacity.
- Ratio < 0.70: Indicates Obstructive Disease (e.g., COPD, Asthma) – air cannot get out fast enough.
- Ratio Normal/High: Indicates Restrictive Disease (e.g., Fibrosis) – lung volume is small, but airways are open.
5. Gas Exchange & Transport (气体交换与运输)
A. Diffusion
Driven by Partial Pressure Gradients ($P_{gas}$).
- Oxygen: Alveoli ($PO_2$ ~100 mmHg) $\rightarrow$ Blood ($PO_2$ ~40 mmHg).
- Carbon Dioxide: Blood ($PCO_2$ ~46 mmHg) $\rightarrow$ Alveoli ($PCO_2$ ~40 mmHg).
B. Oxygen Transport
- 98.5% bound to Hemoglobin (Hb): Oxyhemoglobin ($HbO_2$).
- One Hb molecule binds 4 $O_2$ molecules.
- 1.5% Dissolved in Plasma: Only dissolved $O_2$ contributes to partial pressure.
- Oxygen-Hb Dissociation Curve: Sigmoidal shape.
- Right Shift (Release $O_2$ to tissues): Caused by High $CO_2$, High Acid (Low pH), High Temp, High 2,3-DPG (Bohr Effect).
C. Carbon Dioxide Transport
- Bicarbonate Ion ($HCO_3^-$): ~70% (Major route).
- Equation: $CO_2 + H_2O \rightleftharpoons H_2CO_3 \rightleftharpoons H^+ + HCO_3^-$.
- (Catalysed by Carbonic Anhydrase in RBCs).
- Carbaminohemoglobin: ~23% (Bound to Hb protein, not heme).
- Dissolved in Plasma: ~7%.
6. Control of Breathing (呼吸调节)
Respiratory Centres: Located in the Brainstem (Medulla Oblongata and Pons).
Chemoreceptors (化学感受器)
The primary drive for breathing is $CO_2$ levels (not Oxygen).
-
Central Chemoreceptors (Medulla):
- Detect changes in CSF pH (indirectly measure blood $PCO_2$).
- High arterial $PCO_2$ $\rightarrow$ $CO_2$ crosses blood-brain barrier $\rightarrow$ Lowers pH $\rightarrow$ Stimulates breathing to blow off $CO_2$.
-
Peripheral Chemoreceptors (Carotid & Aortic Bodies):
- Detect changes in arterial $PO_2$, $PCO_2$, and pH.
- Only stimulated by significant hypoxia ($PO_2$ < 60 mmHg).
Summary Table (Physiology Parameters)
| Parameter | Normal Value (Approx) | Notes |
|---|---|---|
| Tidal Volume | 500 mL | Normal breath |
| Respiratory Rate | 12-20 bpm | Breaths per minute |
| Arterial $PO_2$ | 80-100 mmHg | Partial pressure of O2 |
| Arterial $PCO_2$ | 35-45 mmHg | Primary driver of ventilation |
| Blood pH | 7.35 - 7.45 | Regulated by lungs (fast) and kidneys (slow) |
LECTURE23 01 Core Concept 20 Pharmacology of respiratory therapeutics
1. Physiological Control of Airway Smooth Muscle (气道平滑肌的生理调节)
Airway tone is determined by the balance between constriction and relaxation pathways.
A. Parasympathetic Nervous System (副交感神经) - The Dominant Constrictor
- Mechanism: The Vagus nerve releases Acetylcholine (ACh).
- Receptor: ACh binds to Muscarinic M3 receptors on airway smooth muscle.
- Effect: Bronchoconstriction (收缩) and increased mucus secretion.
- Relevance: This is the primary reversible component in COPD (high vagal tone).
B. Sympathetic Nervous System (交感神经) - The Relaxer
- Anatomy: There is very sparse direct sympathetic innervation to airway smooth muscle in humans.
- Mechanism: Instead, circulating Adrenaline (Epinephrine) activates receptors.
- Receptor: Beta-2 ($\beta_2$) Adrenergic receptors are abundant on airway smooth muscle (and immune cells like mast cells).
- Effect: Bronchodilation (舒张) and inhibition of mediator release.
C. NANC System (Non-adrenergic, non-cholinergic)
- Inhibitory (i-NANC): Releases Nitric Oxide (NO) and VIP $\rightarrow$ Bronchodilation.
- Excitatory (e-NANC): Releases Substance P and Neurokinin A $\rightarrow$ Bronchoconstriction (Neurogenic inflammation).
2. Bronchodilators (支气管扩张剂)
A. Beta-2 Adrenoceptor Agonists ($\beta_2$受体激动剂)
The most effective bronchodilators.
Mechanism of Action (MOA):
- Agonist binds to the $\beta_2$ receptor (a GPCR coupled to $G_s$).
- Activates Adenylyl Cyclase (AC).
- Increases intracellular cAMP (cyclic AMP).
- Activates Protein Kinase A (PKA).
- Downstream Effects:
- Lowers intracellular Calcium ($Ca^{2+}$).
- Inhibits Myosin Light Chain Kinase (MLCK).
- Opens Potassium channels ($K^+$) causing hyperpolarization.
- Result: Smooth Muscle Relaxation.
Classification:
- SABA (Short-Acting): Salbutamol (Albuterol), Terbutaline.
- Hydrophilic (亲水性).
- Rapid onset, short duration (4-6h). Used for rescue.
- LABA (Long-Acting): Salmeterol, Formoterol.
- Lipophilic (亲脂性).
- Salmeterol MOA: Has a long lipophilic tail that anchors into an “exosite” near the receptor, allowing the active head to repeatedly bind and unbind. Slow onset, long duration (12h).
- Formoterol MOA: Dissolves in the lipid membrane and slowly leaches out to the receptor. Rapid onset (like SABA) but long duration.
Adverse Effects (Side Effects):
- Tremor (震颤): Activation of $\beta_2$ receptors in skeletal muscle.
- Tachycardia/Palpitations (心动过速): Cross-reactivity with $\beta_1$ receptors in the heart (at high doses) or reflex tachycardia from vasodilation.
- Hypokalaemia (低血钾): Drives $K^+$ into cells.
- Tolerance (Down-regulation): Overuse can lead to receptor internalization.
B. Muscarinic Antagonists (Anticholinergics - 抗胆碱能药物)
Primarily used in COPD, increasingly in Asthma.
Mechanism of Action (MOA):
- Competitively block M3 receptors on airway smooth muscle.
- Inhibit the constricting effect of Acetylcholine (ACh).
- Reduce mucus hypersecretion.
Classification:
- SAMA (Short-Acting): Ipratropium Bromide.
- Non-selective blocker (blocks M1, M2, M3). Blocking M2 (autoreceptor) can potentially increase ACh release, limiting efficacy.
- Duration ~4-6h.
- LAMA (Long-Acting): Tiotropium.
- Kinetic Selectivity: Dissociates very slowly from M3 receptors (long duration >24h) but rapidly from M2 receptors. This makes it superior to Ipratropium.
- Clinical Note: More effective in COPD (where vagal tone is a major factor) than in Asthma (where inflammation is key).
C. Methylxanthines (甲基黄嘌呤类)
- Drugs: Theophylline, Aminophylline (IV form).
- Mechanism of Action (Complex & Multiple):
- PDE Inhibition: Inhibits Phosphodiesterase (PDE3/4) $\rightarrow$ Prevents breakdown of cAMP $\rightarrow$ Sustains bronchodilation.
- Adenosine Antagonism: Blocks Adenosine receptors (which usually cause bronchoconstriction).
- HDAC Activation: Increases Histone Deacetylase activity $\rightarrow$ Reverses steroid resistance (Anti-inflammatory effect).
- Limitations: Narrow Therapeutic Index (requires blood monitoring). Side effects include arrhythmias, seizures, nausea. Metabolised by CYP450 (lots of interactions).
3. Anti-Inflammatory Agents (抗炎药物)
A. Corticosteroids (皮质类固醇) - The Cornerstone of Asthma Tx
Mechanism of Action (Genomic):
Steroids are lipophilic and enter the cell cytoplasm to bind the Glucocorticoid Receptor (GR). The complex moves to the nucleus.
- Transactivation (Switching Genes ON):
- Increases production of Lipocortin (Annexin A1).
- Lipocortin inhibits Phospholipase A2 (PLA2), stopping the Arachidonic Acid cascade (blocking Prostaglandins and Leukotrienes at the source).
- Upregulates $\beta_2$ receptor expression (counteracts tolerance).
- Transrepression (Switching Genes OFF):
- Inhibits transcription factors like NF-$\kappa$B.
- Reduces production of pro-inflammatory cytokines (IL-4, IL-5, TNF-$\alpha$, GM-CSF).
- Reduces recruitment of Eosinophils and T-cells.
Side Effects:
- Local (Inhaled): Oral Candidiasis (Thrush - 鹅口疮), Dysphonia (hoarseness). Counselling: Rinse mouth after use.
- Systemic (Oral/High Dose): Adrenal suppression, Osteoporosis, Diabetes, Hypertension, Growth suppression in children.
B. Leukotriene Receptor Antagonists (LTRAs)
- Drugs: Montelukast, Zafirlukast.
- Pathophysiology: Leukotrienes (CysLTs) are potent constrictors produced by mast cells/eosinophils. They are 1000x more potent than histamine.
- Mechanism: Competitively block the CysLT1 receptor.
- Clinical Use: Oral tablets. Particularly effective for Aspirin-sensitive asthma and Exercise-induced asthma. Add-on therapy.
C. Mast Cell Stabilisers (Chromones)
- Drugs: Sodium Cromoglicate, Nedocromil.
- Mechanism: Stabilise mast cell membranes by blocking chloride channels, preventing degranulation (release of histamine).
- Use: Weak effect. Mainly used in children or mild allergic asthma. Prophylactic only.
D. Biologics (Monoclonal Antibodies - 单克隆抗体)
For severe, refractory eosinophilic asthma.
- Omalizumab (Xolair): Anti-IgE. Binds to free IgE, preventing it from binding to mast cells. Prevents degranulation.
- Mepolizumab / Reslizumab: Anti-IL-5. IL-5 is the major cytokine for Eosinophil survival and activation. Reduces eosinophil counts.
4. Summary Table of Receptors
| Drug Class | Target Receptor | Action | Result |
|---|---|---|---|
| SABA/LABA | $\beta_2$-Adrenergic | Agonist | $\uparrow$ cAMP $\rightarrow$ Relaxation |
| SAMA/LAMA | Muscarinic M3 | Antagonist | Blocks ACh $\rightarrow$ Prevents Constriction |
| Steroids | Glucocorticoid (Nuclear) | Agonist | Gene transcription modulation $\rightarrow$ Anti-inflammatory |
| LTRAs | CysLT1 | Antagonist | Blocks Leukotrienes $\rightarrow$ Prevents Constriction/Inflammation |
| Omalizumab | Circulating IgE | Binder | Prevents Mast Cell Activation |
LECTURE42 01 Core Concept Lecture - Asthma therapeutics
1. Definition & Pathophysiology (定义与病理生理)
Definition
- A chronic inflammatory disorder of the airways (气道慢性炎症).
- Characterized by Reversible airflow obstruction (可逆性气流阻塞).
- Key Symptoms:
- Wheeze (喘息 - 呼气时的高音调哨声).
- Breathlessness (呼吸困难).
- Chest tightness (胸闷).
- Cough (咳嗽 - 尤以夜间或清晨为甚).
Pathophysiology
- Bronchoconstriction (支气管收缩): Smooth muscle contraction leading to narrowing of airways.
- Inflammation (炎症): Oedema (水肿) and mucus hypersecretion (粘液分泌过多).
- Airway Remodelling (气道重塑): Without proper treatment, chronic inflammation leads to permanent structural changes (fibrosis), resulting in irreversible obstruction.
Phases of Asthma Attack
- Early Phase (Immediate): Triggered by allergens (IgE mediated). Mast cells degranulate $\rightarrow$ Histamine/Leukotrienes release $\rightarrow$ Bronchospasm.
- Late Phase (Hours later): Influx of inflammatory cells (Eosinophils, Th2 lymphocytes). Causes edema and mucus plugging. Corticosteroids target this phase.
2. Diagnosis (诊断)
There is a significant divergence between NICE and BTS/SIGN guidelines regarding diagnosis.
NICE Guidelines (Algorithm-based)
Focuses on objective testing first.
- FeNO (Fractional exhaled Nitric Oxide): Measures eosinophilic inflammation.
- Positive if $\ge$ 40 ppb (adults).
- Spirometry (肺量计):
- Obstructive picture: FEV1/FVC ratio < 70%.
- Bronchodilator Reversibility (BDR):
- Improvement in FEV1 of $\ge$ 12% AND $\ge$ 200ml after SABA.
BTS/SIGN Guidelines (Clinical-based)
Focuses on clinical probability.
- High Probability: Typical symptoms + history $\rightarrow$ Trial of treatment (Give inhaled corticosteroids for 6 weeks and review).
- Intermediate Probability: Perform Spirometry/BDR.
- Low Probability: Investigate other causes.
3. Pharmacology: Drug Classes (药物类别)
A. Bronchodilators (支气管扩张剂) - “Relievers”
1. Beta-2 Agonists ($\beta_2$激动剂)
- Mechanism (MOA): Stimulate $\beta_2$ receptors in lung smooth muscle $\rightarrow$ Increase cAMP $\rightarrow$ Relaxation (Bronchodilation).
- SABA (Short-Acting): Salbutamol, Terbutaline.
- Onset: Rapid (<5 min). Duration: 4-6 hours.
- Use: “As needed” (PRN) for symptom relief.
- LABA (Long-Acting): Salmeterol, Formoterol.
- Duration: ~12 hours.
- CRITICAL SAFETY NOTE: LABAs must NEVER be used as monotherapy in asthma. Always combine with ICS to prevent masking inflammation while risk of death increases.
- Formoterol is unique: Rapid onset (can be used for relief in MART therapy) + Long duration.
2. Antimuscarinics (抗胆碱能药物)
- Mechanism: Block M3 muscarinic receptors $\rightarrow$ Inhibit Acetylcholine-induced constriction.
- LAMA (Long-Acting): Tiotropium.
- Use: Add-on therapy in severe asthma (Step 4/5).
- SAMA (Short-Acting): Ipratropium.
- Use: Mainly in Acute Asthma (Nebulised).
3. Methylxanthines
- Drug: Theophylline / Aminophylline.
- Use: Oral add-on (rarely used now due to narrow therapeutic index and interactions).
B. Anti-inflammatories (抗炎药) - “Preventers”
1. Corticosteroids (皮质类固醇)
- Mechanism:
- Enter cell nucleus $\rightarrow$ Bind to Glucocorticoid Response Elements (GRE).
- Upregulate anti-inflammatory proteins (Lipocortin).
- Downregulate pro-inflammatory cytokines (IL-4, IL-5).
- Reduce airway responsiveness.
- ICS (Inhaled): Beclometasone, Budesonide, Fluticasone.
- The cornerstone of asthma maintenance.
- Side Effects: Oral candidiasis (thrush - advise rinsing mouth), hoarse voice.
- OCS (Oral): Prednisolone.
- Use: Acute attacks (Rescue) or Maintenance in Step 5 (Severe).
2. Leukotriene Receptor Antagonists (LTRA)
- Drug: Montelukast.
- Mechanism: Blocks Cysteinyl-Leukotriene receptors (CysLT1) $\rightarrow$ Reduces inflammation and bronchoconstriction.
- Use: Oral tablet, useful for exercise-induced asthma or allergic rhinitis comorbidity.
3. Biologics (Monoclonal Antibodies)
- Omalizumab (Anti-IgE).
- Mepolizumab (Anti-IL5).
- Use: Severe, specialist-managed eosinophilic asthma.
4. Chronic Management: The Stepwise Approach (阶梯治疗)
Based on BTS/SIGN (Adults). The goal is complete control: no daytime symptoms, no night wakening, no limitations.
-
Step 1: Mild Intermittent Asthma
- SABA (Salbutamol) as needed.
- Note: Recent global guidelines (GINA) suggest low dose ICS-formoterol prn even at Step 1 to reduce exacerbation risk, but standard UK practice often starts with SABA.
-
Step 2: Regular Preventer
- Indication: Using SABA > 3 times/week, or night symptoms > 1/week.
- Add Low Dose ICS (e.g., Beclometasone 200-400mcg/day).
-
Step 3: Initial Add-on
- Add LABA (Standard: Fixed-dose combination inhaler, e.g., Seretide or Fostair).
- If LABA helps but control is inadequate: Continue LABA and increase ICS to medium dose.
- If LABA doesn’t help: Stop LABA and try LTRA (Montelukast).
-
Step 4: Persistent Poor Control
- Medium Dose ICS + LABA.
- Consider adding: LTRA, or LAMA (Tiotropium), or Theophylline.
- MART Therapy (Maintenance and Reliever Therapy): Using a combination inhaler containing ICS + Formoterol for both maintenance (twice daily) AND relief (instead of Salbutamol). This is very effective as it increases steroid load automatically when symptoms worsen.
-
Step 5: Severe Asthma
- Refer to specialist.
- High dose ICS.
- Oral Steroids (Prednisolone).
- Biologics (Omalizumab).
5. Acute Asthma Management (急性哮喘管理)
Assessment of Severity
- Moderate: PEF 50-75% best/predicted. Able to speak.
- Severe: PEF 33-50%. Can’t complete sentences. Pulse >110. RR >25.
- Life-Threatening: PEF <33%. Silent chest (no wheeze audible due to no air movement). Cyanosis. Hypotension. Confusion. “33-92-CHEST” (PEF<33, Sat<92, Cyanosis/Hypotension/Exhaustion/Silent Chest/Tachycardia).
Immediate Treatment (“O SHIT” Mnemonic)
- Oxygen: High flow (maintain saturation 94-98%).
- Salbutamol: Nebulised (5mg). Repeat back-to-back.
- Hydrocortisone: IV (or Prednisolone Oral 40-50mg). Steroids are crucial to stop the late-phase reaction.
- Ipratropium: Nebulised (0.5mg). Added to Salbutamol for severe cases.
- Theophylline / Magnesium Sulfate: IV (Senior decision).
6. Inhaler Technique & Adherence (吸入技术与依从性)
Poor technique is a major cause of treatment failure.
- pMDI (Pressurized Metered Dose Inhaler):
- Requires coordination (“Press and breathe”).
- Use with a Spacer (储雾罐): Increases lung deposition, reduces oropharyngeal deposition (less thrush).
- DPI (Dry Powder Inhaler):
- Requires strong inspiratory flow (Breath actuated).
- Examples: Accuhaler, Turbohaler.
- Pharmacist Role: Check technique at every opportunity (Medicine Use Review / NMS).
LECTURE31 01 Core Concept 27 COPD treatment and management
Lecturer: [Refer to Transcript]
1. Definition & Pathophysiology (定义与病理生理)
- Definition: A common, preventable, and treatable disease characterised by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities (usually caused by exposure to noxious particles/gases).
- Key Components:
- Chronic Bronchitis (慢性支气管炎): Inflammation and mucus hypersecretion (“Blue Bloaters”).
- Emphysema (肺气肿): Destruction of alveolar walls, loss of elastic recoil (“Pink Puffers”).
- Reversibility: Unlike Asthma, airflow limitation in COPD is not fully reversible (不可完全逆转).
2. Diagnosis & Assessment (诊断与评估)
A. Diagnosis Criteria
- Spirometry (肺活量测定): Essential for diagnosis.
- Key Metric: Post-bronchodilator FEV1/FVC < 0.70 confirms persistent airflow limitation.
B. Assessment Tools
The goal is to determine the severity of airflow limitation, symptoms, and risk of exacerbations.
1. Severity of Airflow Limitation (GOLD 1-4 Grades):
Based on post-bronchodilator FEV1 (in patients with FEV1/FVC < 0.70):
- GOLD 1 (Mild): FEV1 $\ge$ 80% predicted.
- GOLD 2 (Moderate): 50% $\le$ FEV1 < 80%.
- GOLD 3 (Severe): 30% $\le$ FEV1 < 50%.
- GOLD 4 (Very Severe): FEV1 < 30%.
2. Symptom Assessment:
- mMRC (Modified Medical Research Council Dyspnoea Scale): Assess breathlessness (0–4 scale).
- CAT (COPD Assessment Test): Comprehensive symptom assessment (Score 0–40).
3. The “ABE” Assessment Tool (GOLD 2023 Update):
Used to guide initial pharmacological treatment.
- Group A (Low Symptom, Low Risk): 0–1 exacerbations (no hospital), mMRC 0–1, CAT <10.
- Group B (High Symptom, Low Risk): 0–1 exacerbations (no hospital), mMRC $\ge$2, CAT $\ge$10.
- Group E (Exacerbation Prone - “Any Symptom”): $\ge$2 moderate exacerbations OR $\ge$1 leading to hospitalisation (irrespective of symptoms). Replaces old groups C & D.
3. Pharmacological Management (药物治疗)
Drug Classes (药物类别)
| Class | Acronym | Examples | MOA / Clinical Use |
|---|---|---|---|
| Short-Acting Beta Agonist | SABA | Salbutamol, Terbutaline | Rescue relief (as needed). |
| Short-Acting Muscarinic Antagonist | SAMA | Ipratropium | Rescue relief. |
| Long-Acting Beta Agonist | LABA | Salmeterol, Formoterol, Indacaterol | Maintenance bronchodilation. |
| Long-Acting Muscarinic Antagonist | LAMA | Tiotropium, Umeclidinium, Aclidinium | Maintenance. often superior to LABA in preventing exacerbations. |
| Inhaled Corticosteroids | ICS | Fluticasone, Budesonide | Anti-inflammatory. Never used as monotherapy in COPD. |
Initial Treatment Algorithm (GOLD 2023)
- Group A: A Bronchodilator (short or long-acting).
- Group B: LABA + LAMA (Dual bronchodilation is now preferred over monotherapy for symptomatic patients).
- Group E: LABA + LAMA (Standard) OR LABA + LAMA + ICS (if blood eosinophils $\ge$ 300 cells/$\mu$L).
Role of ICS (吸入性皮质类固醇的作用)
- Indication: Consider if history of hospitalisation for exacerbations, $\ge$2 moderate exacerbations/year, or Blood Eosinophils $\ge$ 300 cells/$\mu$L.
- Contraindication: Avoid if repeated pneumonia events, blood eosinophils < 100 cells/$\mu$L, or history of mycobacterial infection.
- Risk: Increased risk of pneumonia (肺炎).
4. Management Cycle & Follow-up (管理循环与随访)
The Management Cycle: Review $\rightarrow$ Assess $\rightarrow$ Adjust.
Follow-up Pathways
If the patient is still symptomatic or exacerbating despite initial treatment:
-
Dyspnoea Pathway (呼吸困难为主):
- If on Monotherapy (LABA or LAMA) $\rightarrow$ Escalate to LABA + LAMA.
- If on LABA + LAMA $\rightarrow$ Switch inhaler device or molecule; investigate other causes (e.g., heart failure).
-
Exacerbation Pathway (急性加重为主):
- If on Monotherapy $\rightarrow$ Escalate to LABA + LAMA.
- If on LABA + LAMA and Eos $\ge$ 300 $\rightarrow$ Escalate to LABA + LAMA + ICS (Triple Therapy).
- If on LABA + LAMA and Eos < 100 $\rightarrow$ Consider Azithromycin (in former smokers) or Roflumilast (if chronic bronchitis).
5. Acute Exacerbations of COPD (AECOPD - 急性加重)
- Definition: Acute worsening of respiratory symptoms that results in additional therapy.
- Triggers: Viral infections (Rhinovirus, Influenza), bacterial infections, pollution.
- Management:
- Bronchodilators: Increase frequency of SABA (with or without SAMA).
- Systemic Corticosteroids: Prednisolone 40mg for 5 days (shortens recovery time, improves oxygenation).
- Antibiotics: Indicated ONLY if the patient has the 3 Cardinal Symptoms (Anthonisen Criteria):
- Increased dyspnoea (呼吸困难加重)
- Increased sputum volume (痰量增加)
- Increased sputum purulence (脓痰 - Key indication)
- Or if requiring mechanical ventilation.
- Common choice: Amoxicillin, Doxycycline, or Clarithromycin (5-7 days).
6. Non-Pharmacological Management (非药物治疗)
- Smoking Cessation (戒烟): The single most effective intervention to slow the decline in lung function and stop progression.
- Vaccinations: Influenza (Annual), Pneumococcal (PCV20/PPSV23), COVID-19, Tdap/Zoster (GOLD 2023/24 updates).
- Pulmonary Rehabilitation (肺康复): Highly effective for reducing dyspnoea and improving quality of life (Groups B & E).
- Inhaler Technique: Critical check at every visit. Poor technique leads to therapeutic failure.
Summary Table (Review Checklist)
| Feature | COPD | Asthma |
|---|---|---|
| Onset | Usually >40 years | Often childhood |
| Smoking History | Common (>10 pack-years) | Variable |
| Symptoms | Persistent, progressive | Variable, intermittent |
| Reversibility | Never fully reversible | Usually reversible |
| First Line Tx | Bronchodilators (LAMA/LABA) | Anti-inflammatory (ICS) |
| ICS Monotherapy | Contraindicated | Common/Standard |
LECTURE32 01 Core Concept 28 Respiratory infections
1. Core Concepts & Pathophysiology (核心概念与病理)
- Definition: Infection of the lower respiratory tract causing inflammation of the alveolar sacs, which fill with fluid or pus (consolidation).
- Key Pathogen: Streptococcus pneumoniae (肺炎链球菌) is the most common cause.
- Characteristics: Gram-positive, alpha-haemolytic, diplococci (pairs).
- Polysaccharide Capsule: A key virulence factor that protects it from phagocytosis.
- Other Pathogens:
- Haemophilus influenzae (common in COPD).
- Atypical Bacteria (非典型菌): Mycoplasma pneumoniae, Legionella pneumophila (Require macrolides as they lack a cell wall or are intracellular).
- Viruses: Influenza, Rhinovirus, COVID-19.
2. Clinical Presentation (临床表现)
Symptoms (症状)
- Cough: Usually productive (purulent/green/yellow sputum).
- Pleuritic Chest Pain (胸膜炎性胸痛): Sharp pain worsened by breathing.
- Fever & Rigors: Shivering/chills.
- Dyspnoea (呼吸困难).
Signs (体征)
- Tachypnoea (呼吸急促): Respiratory rate > 20 bpm.
- Tachycardia (心动过速).
- Dullness to Percussion (叩诊浊音): Indicates fluid/consolidation in lungs.
- Bronchial Breathing: Harsh breath sounds.
Diagnosis (诊断)
- Chest X-ray (CXR): Gold standard. Shows Lobar Consolidation (大叶性实变).
- Microbiology: Sputum culture, Blood culture.
- Urinary Antigen Test: Specific for S. pneumoniae and Legionella.
- Blood Tests: Elevated CRP (>100 mg/L usually bacterial) and Neutrophilia.
3. Risk Stratification: CURB-65 Score (风险分层)
This is the standard tool used in the UK to determine severity and place of care.
| Acronym | Criteria | Point |
|---|---|---|
| C | Confusion (Abbreviated Mental Test score $\le$ 8/10) | 1 |
| U | Urea > 7 mmol/L (Renal impairment/Dehydration) | 1 |
| R | Respiratory Rate $\ge$ 30 /min | 1 |
| B | Blood Pressure (SBP < 90 or DBP $\le$ 60 mmHg) | 1 |
| 65 | Age $\ge$ 65 years | 1 |
Management based on Score
- Score 0-1 (Low Risk): Treat at Home (Oral antibiotics). mortality <3%.
- Score 2 (Moderate Risk): Consider Hospital admission (Short stay). mortality ~9%.
- Score 3-5 (High Risk): Urgent Hospital admission (Consider ICU). mortality 15-40%.
4. Pharmacological Management (药物治疗)
Principle: Start antibiotics within 4 hours of diagnosis. Duration is typically 5 days for mild/moderate cases.
A. Low Severity (CURB-65 = 0 or 1)
- First Line: Amoxicillin 500mg TDS PO (Oral).
- MOA: Penicillin, inhibits bacterial cell wall synthesis.
- Penicillin Allergy:
- Doxycycline 200mg loading dose then 100mg OD.
- OR Clarithromycin 500mg BD.
B. Moderate Severity (CURB-65 = 2)
- Treatment: Amoxicillin (Oral) + Clarithromycin (Oral).
- Or Doxycycline alone if allergic.
- Rationale: The Macrolide (Clarithromycin) is added to cover Atypical organisms (like Legionella/Mycoplasma) which Penicillins cannot kill.
C. High Severity (CURB-65 = 3-5)
- Treatment: Co-amoxiclav (IV) + Clarithromycin (IV/Oral).
- Rationale: Broad spectrum coverage including beta-lactamase producers (S. aureus, H. influenzae) and atypicals.
- Penicillin Allergy: Levofloxacin (Fluoroquinolone) - Note: Safety concerns regarding tendonitis/aortic aneurysm.
D. Supportive Care
- Oxygen (maintain Saturation > 94%).
- IV Fluids (for dehydration/shock).
- Analgesia (Paracetamol/NSAIDs) for pleuritic pain.
- Stop Smoking: Essential advice.
5. Prevention (预防)
Vaccination
- Pneumococcal Polysaccharide Vaccine (PPV / Pneumovax 23):
- Covers 23 serotypes.
- Target Group: All adults $\ge$ 65 years, and “At Risk” groups (Chronic Heart/Lung/Liver/Kidney disease, Diabetes, Immunosuppression, Asplenia).
- Usually a single lifetime dose (repeat every 5 years only for Asplenia/Kidney disease).
- PCV13 (Prevenar): Conjugate vaccine, part of childhood immunisation.
Influenza Vaccine
- Annual vaccination is crucial as secondary bacterial pneumonia often follows the flu (“Post-viral pneumonia”).
Summary Table (Cheatsheet)
| Severity (CURB-65) | Place of Care | First Line Antibiotic (UK) | Penicillin Allergy |
|---|---|---|---|
| Mild (0-1) | Home | Amoxicillin (Oral) | Doxycycline / Clarithromycin |
| Mod (2) | Hospital | Amoxicillin + Clarithromycin | Doxycycline / Levofloxacin |
| Severe (3-5) | Hospital / ICU | Co-amoxiclav (IV) + Clarithromycin | Levofloxacin |
Clinical Pearl: Always check recent travel history. If a patient has recently stayed in a hotel with air conditioning and presents with pneumonia + hyponatraemia (low sodium) + confusion, suspect Legionella (Legionnaires’ disease) and ensure a Macrolide or Quinolone is used.
LECTURE27 01 Core Concept 24 Inhaled formulations, excipients & testing
Core Goal: To deliver the drug to the correct part of the lung (Targeting) while avoiding the throat (Side effects) and ensuring the formulation is stable and deliverable.
1. Pulmonary Physiology & Deposition Physics (肺生理与沉积物理)
The Target Zones
- Conducting Zone (传导区): Trachea to Terminal Bronchioles. Lined with ciliated epithelium and mucus (Mucociliary escalator clearance).
- Respiratory Zone (呼吸区): Respiratory Bronchioles to Alveoli. Huge surface area (~100 $m^2$), thin barrier. Site of systemic absorption.
- Clearance:
- Upper airways: Mucociliary clearance (swallowed).
- Alveoli: Macrophages (phagocytosis).
Aerodynamic Diameter ($d_a$ - 空气动力学直径)
- Particles are irregular. We describe them as an equivalent sphere of unit density ($1 g/cm^3$) that settles at the same velocity as the particle in question.
- Formula: $d_a = d_g \sqrt{\frac{\rho}{\rho_0} \cdot \frac{1}{\chi}}$
- $d_g$: Geometric diameter.
- $\rho$: Particle density.
- $\chi$: Shape factor (Spheres = 1, Flakes > 1).
- Key implication: A small, heavy particle behaves the same as a large, light particle.
- The “Magic Range”: 1 – 5 $\mu m$ is ideal for deep lung deposition.
Mechanisms of Particle Deposition (颗粒沉积机制)
- Inertial Impaction (惯性撞击):
- Where: Upper airways (Throat/Trachea) & Bifurcations.
- Mechanism: Large particles (>5-10 $\mu m$) or High velocity. Momentum prevents them from following the airstream curve.
- Result: Swallowed (Local side effects, e.g., oral thrush from steroids).
- Gravitational Sedimentation (重力沉降):
- Where: Small airways/Bronchioles (Low airflow velocity).
- Mechanism: Gravity pulls particles down. Governed by Stokes’ Law.
- Optimal size: 1-5 $\mu m$.
- Clinical Tip: This is why we tell patients to “Hold their breath” (increases time for sedimentation).
- Brownian Diffusion (布朗扩散):
- Where: Alveoli.
- Mechanism: Random motion of very small particles (<0.5 $\mu m$).
- Issue: Many are exhaled before they touch the wall.
2. Inhaler Devices & Formulations (装置与制剂)
A. Pressurised Metered Dose Inhalers (pMDIs - 压力定量吸入器)
- Principle: Drug dissolved or suspended in a liquid propellant held under pressure. Actuation releases a metered volume which flash-evaporates, leaving drug particles.
- Excipients:
- Propellants:
- Old: CFCs (Chlorofluorocarbons) - Banned (Ozone layer).
- Current: HFAs (Hydrofluoroalkanes - HFA-134a, HFA-227).
- Co-solvents: Ethanol. HFAs are poor solvents, so ethanol helps dissolve the drug or surfactant.
- Surfactants: Oleic acid, Sorbitan trioleate. Lubricate the valve and stabilise suspensions (prevent caking).
- Propellants:
- Challenges:
- Coordination: Patient must press and breathe simultaneously. Solution: Spacers (储雾罐) or Breath-Actuated pMDIs (Easi-Breathe).
- Cold Freon Effect: The chilling sensation of evaporating propellant hits the back of the throat, causing the patient to stop inhaling.
- Spray Velocity: High velocity leads to high throat deposition (Impaction).
B. Dry Powder Inhalers (DPIs - 干粉吸入器)
- Principle: Breath-actuated. The patient’s inspiratory effort provides the energy to de-agglomerate the powder.
- Formulation Strategies:
- Carrier-Based Systems (Most common):
- Micronised Drug (1-5 $\mu m$): Very cohesive, flows poorly, sticks together.
- Coarse Carrier (e.g., Lactose Monohydrate, 50-100 $\mu m$): Flows well.
- Mechanism: Drug particles adhere to the surface of lactose. During inhalation, turbulence knocks the drug off the carrier. The carrier hits the throat (swallowed), drug goes to lungs.
- Pelletised/Spheroids: Soft aggregates of drug alone (e.g., Bricanyl Turbohaler).
- Carrier-Based Systems (Most common):
- Forces involved:
- Adhesion: Van der Waals, Electrostatic, Capillary forces (Drug sticking to carrier).
- Detachment: Drag force and Lift force (Airflow trying to pull drug off).
- Resistance: DPIs have different internal resistance. High resistance requires lower inspiratory flow rate to generate turbulence.
C. Nebulisers (雾化器)
- Principle: Convert liquid solution/suspension into a continuous mist.
- Types:
- Jet Nebuliser: Uses compressed gas (Bernoulli principle). Noisy, cools the liquid.
- Ultrasonic: Uses piezoelectric crystal. Silent, but heats up (bad for proteins/DNA).
- Vibrating Mesh: Liquid pushed through a mesh. Efficient, portable, expensive.
- Formulation:
- Sterile (Essential).
- Isotonic (Prevent bronchoconstriction).
- pH controlled (>5).
- Preservative-free (Sulfites/Benzalkonium chloride can cause bronchospasm).
3. Quality Control & Testing (质量控制与测试)
Regulatory bodies (BP/USP) require strict testing of aerodynamic performance.
Apparatus (测试仪器)
- Twin Impinger (Glass):
- Simple, two chambers (Upper airway vs Lower airway).
- Limit: Only gives a coarse “Respirable Fraction”. Doesn’t give a full size distribution.
- Andersen Cascade Impactor (ACI):
- 8 stages (Metal plates).
- Air flows through progressively smaller holes, increasing velocity. Particles impact on plates based on inertia.
- Standard: Long history of use.
- Next Generation Impactor (NGI):
- 7 stages + MOC (Micro-Orifice Collector).
- Designed specifically for pharma. Horizontal layout, easy to automate.
- Gold Standard for modern testing.
Key Data Metrics (数据指标)
From the impactor data (Mass of drug on each stage), we calculate:
- Mass Median Aerodynamic Diameter (MMAD): The midpoint diameter (50% of particles by mass are larger, 50% are smaller). Ideally 1-5 $\mu m$.
- Geometric Standard Deviation (GSD): Measures the spread (polydispersity). GSD = 1 is monodisperse (all same size). GSD > 1.2 is polydisperse.
- Fine Particle Dose (FPD): The absolute mass of drug < 5 $\mu m$.
- Fine Particle Fraction (FPF): The percentage of the emitted dose that is < 5 $\mu m$.
- $FPF = \frac{\text{Fine Particle Dose}}{\text{Total Emitted Dose}} \times 100%$
Summary Table: Device Comparison
| Feature | pMDI | DPI | Nebuliser |
|---|---|---|---|
| State | Solution/Suspension + Gas | Solid Powder | Solution/Suspension |
| Actuation | Press & Breathe (Coordination needed) | Breath-Actuated (Patient effort needed) | Continuous breathing |
| Delivery Efficiency | Low (~10-20% lung dep) without spacer | Variable (depends on inspiratory flow) | High volume delivery possible |
| Portability | High | High | Low (usually) |
| Propellant | Yes (HFA) | No | No |
Core Concept - Science & Formulations
LECTURE21 01 Core Concept 18 Sterilisation processing
Lecturer: Dr David Allison
1. Introduction & Definitions
Chinese Term: 介绍与定义
A. Approaches to Manufacturing
- Terminal Sterilisation (终端灭菌):
- Product is assembled, packaged, and then sterilised in its final container.
- Preferred method if the product is heat stable.
- Aseptic Processing (无菌工艺):
- Product is assembled from sterile components under controlled “clean” conditions (free of microorganisms).
- Used when the product cannot withstand terminal sterilisation (e.g., heat-labile antibiotics).
B. Definitions
- Sterile (无菌): Free of viable microorganisms (无活微生物).
- Sterilisation (灭菌): The process of killing or removing all viable microorganisms.
Key Concept: A simple product (e.g., antibiotic vial) might require multiple sterilisation steps:
- Solution $\rightarrow$ Filtration (Heat labile).
- Vial $\rightarrow$ Dry Heat.
- Stopper $\rightarrow$ Autoclaving or Gamma Radiation.
2. Traditional Sterilisation Methods
Chinese Term: 传统灭菌方法
Methods are classified into two categories:
- Removal (去除): Filtration.
- Destructive (破坏/杀灭): Heat, Chemical (Gas), Radiation.
A. Filtration (Removal Mechanism)
Chinese Term: 过滤灭菌
- Mechanism: Passage of fluid (liquid/gas) across a filter to remove contaminating solutes/microbes.
- Pore Size Requirement: 0.22 $\mu m$ (or smaller) is required to remove bacteria.
Filter Types Comparison:
| Feature | Depth Filters (深层过滤器) | Screen (Absolute) Filters (膜/筛网过滤器) |
|---|---|---|
| Pore Size | Non-fixed, variable (不固定) | Uniform, fixed (e.g., 0.22 $\mu m$) |
| Mechanism | Inertial impaction (trapped inside) | Direct interception (lodged on surface) |
| Capacity | High retentative capacity | Easily blocked |
| Durability | Robust, cheap | Fragile, expensive (5-10x cost) |
| Sterility | Cannot guarantee sterility | Can produce sterile filtrate |
3. Inactivation Kinetics (The Maths of Killing)
Chinese Term: 灭菌动力学
When microbes are exposed to a lethal agent (heat/radiation), they die at a predictable rate.
A. The Kill Curve
- Linear Plot: Shows an asymptote curve (fixed proportion killed per time unit). Never technically hits zero.
- Semi-log Plot (Log Survivors vs. Time): Produces a straight line.
- This allows us to calculate death rates.
B. D-Value (Decimal Reduction Time)
Chinese Term: D值 (十倍减少时间)
- Definition: The time taken, at a fixed temperature (or dose), to reduce the microbial population by 90% (i.e., a 1-log cycle reduction).
- Significance: Measures the resistance of an organism. Higher D-value = More resistant organism.
C. Sterility Assurance Level (SAL)
Chinese Term: 无菌保证水平
- Since “zero” survivors cannot be plotted on a log scale, we define a statistical probability of sterility.
- Target SAL: $10^{-6}$ (Probability of 1 non-sterile unit in 1,000,000 units).
- Calculation:
- If Initial Bioburden = $10^2$
- Target SAL = $10^{-6}$
- Total Reduction Needed = 8 log cycles ($2 - (-6) = 8$).
- Total Processing Time = $8 \times \text{D-value}$.
Factors affecting Sterilisation Time:
- D-value: Higher resistance requires longer time.
- Bioburden (生物负载): Higher initial population requires longer time.
4. Destructive Methods Details
A. Heat Sterilisation
Chinese Term: 热灭菌
1. Moist Heat (Steam) - Autoclave (湿热/高压蒸汽灭菌):
- Mechanism: Protein coagulation and hydrolysis (蛋白质凝固和水解).
- Conditions: Steam under pressure (temps > $100^\circ\text{C}$).
- Pros: Rapid, safe, reliable, easy to monitor. Most widely used.
- Autoclave Cycle Stages:
- Air Removal (Crucial! Air pockets prevent reaching $>100^\circ\text{C}$).
- Heating.
- Holding Period (Sterilisation phase).
- Cooling.
- Drying.
- Common Pharmacopoeial Cycles:
- $121^\circ\text{C}$ for 15 mins (Aqueous products, standard cycle).
- $134^\circ\text{C}$ for 3 mins (Porous loads, surgical dressings).
2. Dry Heat (干热灭菌):
- Mechanism: Oxidative processes (氧化作用).
- Uses: Glassware, oils, dry powders (items that steam can’t penetrate or would damage).
- Conditions: Higher temperatures and longer times than moist heat (e.g., $160^\circ\text{C}$ for 2 hrs).
B. Ethylene Oxide (EtO)
Chinese Term: 环氧乙烷灭菌
- Type: Chemical Gas Sterilant.
- Mechanism: Alkylation of proteins and nucleic acids (烷基化作用).
- Uses: Heat-sensitive Single-use medical devices (syringes, catheters).
- Critical Parameters: Concentration, Temperature, Humidity, Time.
- Disadvantages:
- Toxic residues (requires desorption/aeration).
- Explosive gas.
- Harder to validate than heat.
- Biological Indicator: Bacillus subtilis (spores) - used to validate the process because they are highly resistant to EtO.
C. Radiation (Briefly mentioned)
- Ionising Radiation (Gamma): Uses Cobalt-60 isotope. Good for dry medical devices.
- Lecturer Note: “There will not be an exam question based on radiation.”
5. Alternative Technologies
Chinese Term: 新型/替代技术
- X-Ray Irradiation: Ionising, low power, used for contact lenses.
- Pulsed Light: Broad spectrum white light (UV content), surface sterilisation.
- Microwaves: Intense heating, short cycles. Solutions/Contact lenses.
- Gas Plasma (气体等离子体):
- Mixture of ions/free radicals (e.g., from $H_2O_2$).
- Advantage: Safer alternative to EtO (non-explosive, no toxic residues).
- Used for medical devices.
6. Quality Assurance & Testing
Chinese Term: 质量保证与测试
How do we prove a product is sterile?
A. Bioburden Estimation
- Definition: The number of microorganisms on/in a product before sterilisation.
- Purpose: Determines the challenge level to calculate the required dose/time.
B. Test for Sterility vs Test of Sterility
- Test for Sterility: Testing the end product (destructive test on a sample batch). Answer is Pass/Fail.
- Test of Sterility: Testing performed during validation/development. Exposing product to a fraction of the process to determine kill rates (D-values).
C. Pyrogen Testing (Endotoxins)
Chinese Term: 热原 (内毒素) 检测
- Pyrogen: Fever-causing substance.
- Main Source: Lipid A component of Lipopolysaccharide (LPS) from the outer membrane of Gram-negative bacteria.
- Problem: Bacteria can be killed (sterile), but dead cell fragments (Endotoxins) remain and can be fatal if injected.
The LAL Test (鲎试剂试验):
- Full Name: Limulus Amebocyte Lysate.
- Source: Blood of the Horseshoe Crab (Limulus polyphemus).
- Mechanism: In the presence of Endotoxin, the lysate forms a Gel Clot (凝胶).
- Types:
- Gel Clot: Simple +/- result (Clot forms = Positive for endotoxin).
- Chromogenic: Colour change, allows quantification (measuring intensity).
Summary Checklist
- [ ] Can you define $D_{value}$ and $SAL$ ($10^{-6}$)?
- [ ] Do you know the difference between Depth and Screen filters?
- [ ] Can you list the 4 stages of an autoclave cycle?
- [ ] Why is Ethylene Oxide dangerous? (Explosive/Toxic residues).
- [ ] What is the LAL test used for? (Detecting Lipid A/Endotoxin from Gram -ve bacteria).
LECTURE33 01 Core Concept 29 Particle Sizing and size distribution
1. Why Measure Particle Size? (为什么要测量粒径?)
Particle size influences critical pharmaceutical properties:
- Dissolution Rate (溶出速率): Smaller particles = larger surface area = faster dissolution (Noyes-Whitney Equation).
- Bioavailability (生物利用度): Faster dissolution often leads to better absorption.
- Stability (稳定性): In suspensions, larger particles settle faster (Stokes’ Law). Ostwald ripening can occur in fine suspensions.
- Processability (加工性能): Affects flowability (crucial for tableting) and mixing homogeneity.
2. Describing Particle Size (粒径的描述)
Since particles are irregular, we measure a property (e.g., volume, settling speed) and relate it to a sphere that would produce the same result.
- Equivalent Sphere Diameter: The diameter of a sphere that behaves the same way as the particle in the chosen measurement method.
- Volume Equivalent Diameter ($d_v$): Sphere with the same volume.
- Stokes’ Diameter ($d_{st}$): Sphere with the same settling velocity.
- Projected Area Diameter ($d_a$): Sphere with the same projected area (Microscopy).
3. Measurement Techniques (测量技术)
A. Sieving (筛分法)
- Range: Coarse particles (> 50 $\mu m$ typically, down to 38 $\mu m$).
- Method: Mechanical agitation of nested sieves.
- Pros: Simple, cheap, robust.
- Cons: Low resolution, cannot measure sprays/emulsions, can cause attrition (particles breaking).
B. Microscopy (显微镜法)
- Range: $1 \mu m$ - $150 \mu m$ (Optical).
- Method: Direct observation.
- Distribution: Gives a Number Distribution (counts individual particles).
- Pros: Allows visualisation of particle shape (agglomerates vs primary particles).
- Cons: Slow, examines small sample size (poor representation), 2D projection only.
C. Laser Diffraction (激光衍射法 - Industry Standard)
- Range: Wide range ($0.02 \mu m$ - $2000 \mu m$).
- Method: Particles pass through a laser beam; light scatters at angles inversely proportional to particle size (Large particles $\to$ Small angles; Small particles $\to$ Large angles).
- Theory: Uses Mie Theory (requires refractive index) or Fraunhofer approximation.
- Distribution: Gives a Volume Distribution (equivalent to mass if density is constant).
- Pros: Fast, reproducible, wide dynamic range.
D. Dynamic Light Scattering (DLS) (动态光散射)
- Range: Sub-micron / Nanoparticles (< $1 \mu m$).
- Method: Measures Brownian motion. Smaller particles move faster.
- Result: Hydrodynamic radius.
4. Data Analysis & Distributions (数据分析与分布)
Number vs. Volume Weighting (数量分布 vs 体积分布)
- Number Distribution: All particles have equal weighting (1 particle = 1 count). Example: Microscopy.
- Volume/Mass Distribution: Larger particles have massive weighting because Volume $\propto r^3$.
- Clinical Note: A few large lumps in an IV emulsion might be negligible by number (0.01%) but could constitute 90% of the volume and cause an embolism. Laser diffraction (Volume) is safer for detecting these large tails.
Key Parameters (关键参数)
- $D_{10}, D_{50}, D_{90}$: Percentiles based on the cumulative distribution (Undersize).
- $D_{v50}$ (Median): 50% of the sample volume is smaller than this size.
- $D_{v90}$: 90% is smaller (indicates the coarse end of the distribution).
- $D_{v10}$: 10% is smaller (indicates the fine end).
- Span (Width of distribution):
$$\text{Span} = \frac{D_{90} - D_{10}}{D_{50}}$$- A smaller span indicates a narrower (more monodisperse) distribution.
Mean Diameters (平均径)
- $D[4,3]$ (Volume Moment Mean): Sensitive to large particles. Similar to the centre of gravity of the volume distribution.
- $D[3,2]$ (Sauter Mean Diameter): Surface area moment mean. Relevant for dissolution and bioavailability studies (surface sensitive).
5. Summary Checklist (复习清单)
| Method | Range | Distribution Type | Key Feature |
|---|---|---|---|
| Sieving | >50 $\mu m$ | Mass | Simple, measures “sieve diameter” (width). |
| Microscopy | 1-150 $\mu m$ | Number | Sees shape; slow; 2D only. |
| Laser Diffraction | 0.02-2000 $\mu m$ | Volume | Fast; standard for most drugs; assumes spherical. |
| DLS | <1 $\mu m$ (Nano) | Intensity/Volume | Measures Brownian motion; for nanoparticles. |
- [ ] Can you calculate Span? Formula: $(D_{90} - D_{10}) / D_{50}$.
- [ ] Why convert Number to Volume? To understand the mass contribution of large particles. A $10\mu m$ particle has $1000 \times$ the volume of a $1\mu m$ particle.
LECTURE6 01 Core Concept 3 Mass Spectrometry of medicines and drug substances
1. Core Principles (核心原理)
Definition & Function
- Mass Spectrometry (MS) is an analytical technique used to measure the mass-to-charge ratio ($m/z$) of ions.
- It acts effectively as a “molecular weighing scale” for atoms and molecules.
- Key Output: A mass spectrum (plot of intensity vs. $m/z$).
The “Black Box” Components (仪器组件)
A standard MS system consists of five main stages:
- Sample Inlet (进样系统): Introduces the sample (solid, liquid, or vapour).
- Ion Source (离子源): Converts neutral molecules into charged ions (Ionisation).
- Mass Analyser (质量分析器): Separates ions based on their $m/z$ ratio.
- Detector (检测器): Counts the ions and measures signal intensity.
- Data System: Processes signals into a spectrum.
Critical Requirement - High Vacuum (高真空):
The entire system (Source $\to$ Detector) operates under a high vacuum ($10^{-5}$ to $10^{-7}$ torr). This prevents ions from colliding with air molecules, which would scatter them and prevent them from reaching the detector.
2. Ionisation Techniques (电离技术)
The choice of ionisation determines whether you see the whole molecule (Molecular Ion) or structural fragments.
A. Electron Impact (EI) - Hard Ionisation (硬电离)
- Mechanism: High-energy electrons (70eV) bombard the sample in the vapour phase.
- Result: Extensive fragmentation (碎片化) occurs.
- Application:
- Provides a “fingerprint” for structural identification.
- Used in GC-MS (Gas Chromatography-MS) for volatile, thermally stable drugs.
- Limitation: Often destroys the Molecular Ion ($M^+$), making it hard to determine molecular weight.
B. Chemical Ionisation (CI) - Softer Ionisation (较软电离)
- Mechanism: Uses a reagent gas (e.g., methane, ammonia) to transfer a proton to the analyte.
- Result: Less fragmentation; typically observes the protonated molecular ion $[M+H]^+$.
- Application: Confirming molecular weight when EI fragments too much.
C. Electrospray Ionisation (ESI) - Soft Ionisation (软电离)
- Mechanism: Sample is sprayed from a capillary at high voltage; solvent evaporates, leaving charged ions.
- Result: Very little fragmentation. Can produce multiply charged ions ($[M+nH]^{n+}$).
- Clinical Relevance:
- The standard interface for LC-MS (Liquid Chromatography-MS).
- Essential for analysing biologicals (proteins, peptides, monoclonal antibodies) because it allows large masses to be detected within the range of standard analysers.
D. MALDI (Matrix Assisted Laser Desorption Ionisation)
- Mechanism: Sample is mixed with a matrix and hit with a laser.
- Application: Large biomolecules (polymers, proteins). Usually singly charged ions.
3. Mass Analysers (质量分析器)
After ionisation, ions are separated by their $m/z$ ratio.
| Analyser Type | Mechanism | Key Features |
|---|---|---|
| Magnetic Sector | Uses a magnetic field to bend ion paths. | Historical standard; high resolution but slow and bulky. |
| Quadrupole (四极杆) | Uses 4 parallel rods with oscillating voltages. | The “Workhorse” of pharma labs. Cheap, robust, fast. Acts as a mass filter. |
| Time of Flight (TOF) | Measures time taken for ions to drift down a flight tube. | Unlimited mass range; extremely fast; high sensitivity. Ideal for biomolecules. |
4. Analysis & Interpretation (谱图解析)
Resolution (分辨率)
- Low Resolution (Unit Mass): Can distinguish $m/z$ 200 from 201. Good for general confirmation.
- High Resolution (Accurate Mass): Can distinguish $m/z$ 28.0187 ($N_2$) from 28.0061 ($CO$).
- Clinical Relevance: Essential for determining elemental composition and identifying unknown impurities or metabolites.
Isotope Patterns (同位素模式)
Elements exist as mixtures of isotopes, creating characteristic patterns in the spectrum.
- Chlorine (Cl): Exists as $^{35}Cl$ and $^{37}Cl$ in a 3:1 ratio.
- Pattern: Look for two peaks separated by 2 mass units with intensities of 100% and 33%.
- Bromine (Br): Exists as $^{79}Br$ and $^{81}Br$ in a 1:1 ratio.
- Pattern: Look for two peaks separated by 2 mass units of roughly equal height (“Twin Towers”).
- Carbon ($^{13}C$): 1.1% natural abundance. Creates a small “satellite” peak at $M+1$.
Fragmentation Rules
- Nitrogen Rule (氮规则):
- Odd Molecular Weight = Odd number of Nitrogen atoms.
- Even Molecular Weight = Even (or zero) Nitrogen atoms.
- Stevenson’s Rule: Fragmentation favours the formation of the most stable cation (e.g., tertiary carbocations > primary).
5. Summary: Pharmaceutical Applications
| Technique | Coupling | Sample Type | Primary Use in Pharma |
|---|---|---|---|
| EI-MS | GC-MS | Volatile, Thermally Stable | Identification of raw materials, residual solvents, volatile impurities. |
| ESI-MS | LC-MS | Polar, Non-volatile, Labile | Bioanalysis (drugs in plasma), Peptide mapping, Metabolite ID. |
| MALDI | N/A (Solid) | High MW Biomolecules | QC of large proteins/polymers. |
6. Exam Focus / Self-Check
- [ ] Can you identify a Chlorine or Bromine atom just by looking at the mass spectrum isotope pattern?
- [ ] Explain why a vacuum is necessary in MS.
- [ ] Distinguish between “Hard” (EI) and “Soft” (ESI) ionisation and when to use each.
- [ ] Why is ESI preferred for biological drugs (proteins)? (Answer: Multiple charging brings high mass into detectable range).
LECTURE13 01 Core Concept 11 NMR spectroscopy of drug substances
1. Core Principles (核心原理)
The Basis of NMR
- Nuclear Spin (核自旋): Certain nuclei behave like tiny magnets. This property is required for NMR.
- Condition: Nuclei must have an odd mass number or odd atomic number to possess spin.
- Pharma-relevant Nuclei: $^1H$ (Proton), $^{13}C$ (Carbon-13), $^{19}F$ (Fluorine), $^{31}P$ (Phosphorus).
- Non-active: $^{12}C$ and $^{16}O$ do not have spin and are invisible in NMR.
The Mechanism
- Magnetic Field ($B_0$): Without a field, nuclear spins are random. In a strong external magnetic field, they align with (Alpha $\alpha$, lower energy) or against (Beta $\beta$, higher energy) the field.
- Resonance (共振): We apply Radiofrequency (RF) radiation. When the RF frequency matches the energy gap ($\Delta E$) between $\alpha$ and $\beta$ states, the nucleus “flips” spin. This absorption of energy is resonance.
- Relaxation: The nucleus returns to the ground state, emitting a signal (FID) which is processed into a spectrum.
2. Interpreting the Proton NMR Spectrum ($^1H$-NMR)
Interpretation relies on three main parameters: Position, Intensity, and Shape.
A. Chemical Shift (Position) - $\delta$ (ppm) (化学位移)
- Definition: Indicates the electronic environment of the proton. Measured relative to a reference standard, TMS (Tetramethylsilane), set at 0 ppm.
- Shielding vs. Deshielding (屏蔽与去屏蔽):
- Shielded (High field/Upfield): High electron density around the nucleus shields it from the external magnet. Signals appear at lower ppm (right side).
- Example: Saturated alkanes ($CH_3$, $CH_2$) $\approx$ 0.9 - 1.5 ppm.
- Deshielded (Low field/Downfield): Electronegative atoms (O, N, Halogens) pull electrons away. The nucleus feels the magnet more strongly. Signals appear at higher ppm (left side).
- Example: Aldehyde protons ($\approx$ 9-10 ppm), Carboxylic acids ($\approx$ 10-12 ppm).
- Shielded (High field/Upfield): High electron density around the nucleus shields it from the external magnet. Signals appear at lower ppm (right side).
- Aromatic Ring Current: Circulating electrons in benzene rings create a magnetic field that reinforces the external field, causing strong deshielding ($\approx$ 6.5 - 8 ppm).
B. Integration (Intensity) (积分)
- Rule: The area under the peak is directly proportional to the number of protons contributing to that signal.
- Usage: Used to determine the ratio of H atoms in the molecule (e.g., a ratio of 3:2:3 suggests a $CH_3-CH_2-CH_3$ fragment).
C. Spin-Spin Splitting (Shape) (自旋-自旋裂分)
- Cause: Protons are influenced by the magnetic alignment of neighbouring protons (on adjacent carbons, typically 3 bonds away).
- The $n + 1$ Rule: If a proton has $n$ equivalent neighbours, its signal splits into $n + 1$ peaks.
- Multiplicity Patterns:
- Singlet (s): 0 neighbours (e.g., isolated $CH_3$ or $OH$).
- Doublet (d): 1 neighbour ($1:1$ intensity).
- Triplet (t): 2 neighbours ($1:2:1$ intensity).
- Quartet (q): 3 neighbours ($1:3:3:1$ intensity).
- Multiplet (m): Complex splitting pattern.
- Coupling Constant ($J$): The distance (in Hz) between split peaks. It is constant regardless of the magnetic field strength and provides info on connectivity.
Note on Labile Protons: Protons on O or N (OH, NH) often appear as broad singlets and do not split neighbouring protons due to rapid exchange with the solvent.
3. Practical Considerations
Solvents (溶剂)
- Problem: Common organic solvents contain Hydrogen, which would swamp the drug’s signal.
- Solution: Use Deuterated Solvents (氘代溶剂) where Hydrogen ($^1H$) is replaced by Deuterium ($^2H$). Deuterium has a different resonance frequency and is “invisible” in $^1H$-NMR.
- Common Examples:
- $CDCl_3$ (Deuterated Chloroform) - Most common.
- $DMSO-d_6$ (Deuterated Dimethyl Sulfoxide).
- $D_2O$ (Deuterium Oxide/Heavy Water).
4. Carbon-13 NMR ($^{13}C$-NMR)
- Abundance: $^{13}C$ is only 1.1% natural abundance (unlike 99% for $^1H$). Signals are much weaker and require more scans.
- Range: Larger chemical shift range (0 - 220 ppm).
- Decoupling: Spectra are usually Proton Decoupled.
- Result: All carbon signals appear as Singlets. There is no splitting.
- Integration: Generally not used because relaxation times vary greatly; peak height does not reliably represent carbon count.
5. Summary Table: Typical Chemical Shifts ($^1H$)
| Proton Type | Structure | Approx. Shift ($\delta$ ppm) | Key Feature |
|---|---|---|---|
| Alkyl | $R-CH_3$ | 0.9 - 1.5 | Upfield (Shielded) |
| Allylic | $C=C-CH_3$ | 1.7 - 2.5 | Next to double bond |
| Alpha to Carbonyl | $O=C-CH$ | 2.0 - 2.7 | Deshielded by C=O |
| Electronegative Adj. | $O-CH$, $Cl-CH$ | 3.0 - 4.5 | Deshielded by O/Halogen |
| Alkenyl | $C=CH$ | 4.5 - 6.5 | Double bond region |
| Aromatic | $Ar-H$ | 6.5 - 8.0 | Ring Current Effect |
| Aldehyde | $O=C-H$ | 9.0 - 10.0 | Very downfield |
| Carboxylic Acid | $O=C-OH$ | 10.0 - 12.0 | Most deshielded |
6. Exam Focus (考试重点)
- [ ] Identify the Solvent: Can you explain why $CDCl_3$ is used instead of $CHCl_3$? (Answer: To avoid massive solvent proton peaks interfering with the sample) .
- [ ] Predict Splitting: Given a structure like Ethanol ($CH_3CH_2OH$), predict the splitting:
- $CH_3$: Triplet (2 neighbours on $CH_2$).
- $CH_2$: Quartet (3 neighbours on $CH_3$).
- [ ] Reference Standard: What is TMS? (Tetramethylsilane, defined as 0 ppm, inert, volatile) .
- [ ] Structure Elucidation: Be prepared to match a simple spectrum to a drug structure (e.g., Paracetamol or Aspirin) by counting protons (Integration) and checking neighbours (Splitting).
LECTURE22 01 Core Concept 19 NMR spectroscopy of drug substances 2
Lecturer:
1. Coupling Constants ($J$ Values) - 偶合常数
The Coupling Constant ($J$) provides critical information about the connectivity and stereochemistry of a molecule.
- Definition: The distance between the split peaks in a multiplet, measured in Hertz (Hz).
- Key Feature: unlike chemical shift ($\delta$), the $J$ value is independent of the external magnetic field strength ($B_0$). A 7 Hz doublet on a 300 MHz instrument is still 7 Hz on a 600 MHz instrument.
Stereochemistry & The Karplus Curve (立体化学与Karplus曲线)
The magnitude of the vicinal coupling constant ($^3J$) depends on the dihedral angle (二面角) between the two C-H bonds.
- Karplus Relationship:
- 90° Angle: $J \approx 0$ Hz (No splitting).
- 0° or 180° Angle: Maximum coupling ($J$ is large).
- Application in Alkenes (烯烃):
- Cis-alkenes ($Z$): Protons are closer (angle $\approx$ 0°), typically $J \approx 10$ Hz.
- Trans-alkenes ($E$): Protons are anti-periplanar (angle $\approx$ 180°), typically $J \approx 16$ Hz.
- Exam Tip: Use $J$ values to distinguish geometric isomers of drugs.
- Aromatic Systems (芳香环):
- Ortho ($J_{ortho}$): $\approx$ 8 Hz (Strong coupling).
- Meta ($J_{meta}$): $\approx$ 2 Hz (Weak/Fine splitting).
- Para ($J_{para}$): $< 1$ Hz (Often not visible).
2. Identifying Labile Protons: The $D_2O$ Shake (重水交换)
Signals from protons attached to heteroatoms (OH, NH, SH, COOH) can be broad or confusing.
- Mechanism: These protons are “labile” (acidic) and exchange rapidly with solvent protons.
- Method:
- Run standard $^1H$ NMR.
- Add Deuterium Oxide ($D_2O$) and shake the tube.
- Result: The labile $H$ is replaced by $D$ ($R-OH \rightarrow R-OD$). Since Deuterium is invisible in $^1H$ NMR, the signal disappears.
- Utility: Confirms the presence of Alcohol, Amine, or Carboxylic acid functional groups.
3. Carbon-13 NMR ($^{13}C$ NMR) - 碳谱
Key Differences from $^1H$ NMR
| Feature | Proton ($^1H$) | Carbon ($^{13}C$) | Notes |
|---|---|---|---|
| Natural Abundance | ~99% | 1.1% | $^{13}C$ is a “dilute” spin system; $^{12}C$ is invisible. |
| Sensitivity | High | Low | Requires more sample and longer acquisition times (more scans). |
| Chemical Shift | 0–14 ppm | 0–220 ppm | Greater dispersion; less peak overlap. |
| Coupling | Yes (H-H) | No (Decoupled) | Spectra appear as singlet lines. |
Interpretation Rules
- Proton Decoupling (质子去偶): Standard $^{13}C$ spectra are run in “broadband decoupled” mode to remove C-H splitting. Every chemically equivalent Carbon appears as a single sharp line.
- No Integration: Peak height does not strictly correlate with the number of carbons (due to relaxation time differences), so we do not integrate $^{13}C$ signals.
- Shift Regions:
- 0–50 ppm: Aliphatic ($CH_3, CH_2, CH$).
- 100–160 ppm: Aromatic / Alkenes.
- 160–220 ppm: Carbonyls ($C=O$), specifically Ketones/Aldehydes (>190 ppm) and Acids/Esters (~170 ppm).
4. Advanced Structural Techniques
DEPT-135 (Distortionless Enhancement by Polarization Transfer)
A sequence used to distinguish between $CH_3$, $CH_2$, $CH$, and Quaternary Carbons ($C_q$).
| Carbon Type | DEPT-135 Signal Phase |
|---|---|
| $CH$ and $CH_3$ | Positive (Up/Normal) |
| $CH_2$ | Negative (Inverted/Down) |
| Quaternary ($C_q$) | Invisible (No signal) |
- Note: By comparing the standard $^{13}C$ spectrum (shows all C) with the DEPT-135, you can identify the “missing” peaks as Quaternary carbons (e.g., carbonyls or substituted ring carbons).
2D NMR (二维核磁)
Used when 1D spectra are too crowded or complex.
- COSY (Correlation Spectroscopy): Shows which Protons are coupling to each other ($H-H$ correlation). Used to trace the carbon skeleton connectivity.
- HSQC / HMQC: Shows which Proton is attached to which Carbon ($H-C$ correlation).
5. Clinical Relevance: Magnetic Resonance Imaging (MRI) - 核磁共振成像
MRI is essentially NMR spectroscopy applied to the water content of the human body.
- Mechanism:
- Detects protons in water ($H_2O$) and fat within tissues.
- Uses a massive superconducting magnet (typically 1.5T to 3T).
- Non-invasive and uses non-ionising radiation (safer than CT/X-rays).
- Contrast ($T_1$ and $T_2$ Relaxation):
- Different tissues (muscle, fat, cerebrospinal fluid, tumour) contain water in different physical environments.
- The Relaxation Times ($T_1$ and $T_2$)—the time it takes for spins to return to equilibrium—differ between these tissues, creating image contrast.
- Contrast Agents:
- Gadolinium ($Gd^{3+}$): A paramagnetic metal used to alter the relaxation time of water protons nearby, highlighting blood vessels or tumours.
6. Exam Focus / Summary Checklist
- [ ] Calculate $J$: If peaks are at 3000 Hz and 3007 Hz, $J = 7$ Hz. This value is constant regardless of whether the machine is 300 MHz or 600 MHz.
- [ ] Identify Isomers: Trans-alkene = Large $J$ (~16Hz); Cis-alkene = Medium $J$ (~10Hz).
- [ ] Labile Protons: If a peak disappears after adding $D_2O$, it is likely an $-OH$ or $-NH$.
- [ ] DEPT Interpretation:
- Peak pointing DOWN = $CH_2$.
- Peak pointing UP = $CH$ or $CH_3$.
- Peak Missing (vs normal spectrum) = Quaternary $C$.
LECTURE24 01 Core Concept 21 Pharmaceutical analysis 1
Core Concept: Ensuring medicines are safe, effective, and of high quality through rigorous testing and systems.
1. Quality Assurance vs. Quality Control (QA 与 QC 的区别)
This is a fundamental concept in the pharmaceutical industry.
Quality Assurance (QA - 质量保证)
- Definition: The sum total of the organised arrangements made with the object of ensuring that medicinal products are of the quality required for their intended use.
- Focus: Prevention (预防).
- Scope: It is a wide-ranging concept covering all matters that individually or collectively influence the quality of a product. It involves the design of the system.
- Key Idea: “Quality is built into the product, not tested into it.” (GMP principles).
Quality Control (QC - 质量控制)
- Definition: That part of GMP concerned with sampling, specifications, and testing.
- Focus: Detection (检测).
- Scope: Documentation, sampling, and release procedures. It ensures that materials are not released for use, nor products released for sale, until their quality has been judged to be satisfactory.
- Key Idea: The actual testing of the raw materials and finished products.
2. Regulatory Framework & Standards (法规与标准)
Pharmacopoeias (药典)
Official publications containing quality standards for medicinal products.
- BP (British Pharmacopoeia): The standard in the UK.
- USP (United States Pharmacopeia): US standard.
- Ph. Eur. (European Pharmacopoeia): European standard.
- JP (Japanese Pharmacopoeia).
ICH Guidelines (国际协调理事会指南)
The International Council for Harmonisation (ICH) brings together regulatory authorities and pharma industry to discuss scientific and technical aspects of drug registration.
- Q-Series (Quality Guidelines): Most relevant to analysis.
- Q1: Stability (稳定性).
- Q2: Analytical Validation (分析方法验证) - Crucial for ensuring your method works.
- Q3: Impurities (杂质).
- Q6: Specifications (质量标准).
3. Types of Analysis (分析类型)
A. Qualitative Analysis (定性分析)
- Question: “What is it?” (Identification).
- Methods: IR Spectroscopy, Melting Point, Colour tests.
B. Quantitative Analysis (定量分析)
- Question: “How much is there?” (Assay).
- Methods: Titration, HPLC, UV-Vis.
- Limit Tests: A semi-quantitative test to ensure impurities (e.g., heavy metals, chlorides) are below a certain limit.
C. Classical vs. Instrumental Methods
- Classical (Wet Chemistry): Titrimetry, Gravimetry.
- Pros: Absolute methods (don’t always need a standard), cheap, high precision for macro amounts.
- Cons: Slow, not sensitive enough for trace analysis.
- Instrumental: Chromatography (HPLC, GC), Spectroscopy (UV, IR, NMR).
- Pros: Sensitive, selective, fast, can measure trace amounts.
- Cons: Expensive, requires reference standards.
4. Titrimetry (Volumetric Analysis - 滴定分析)
Despite being “old-school,” titration is still widely used in pharmacopoeias for Assay (content determination) of raw materials because it offers high precision.
Principles
- Stoichiometry: The reaction between the analyte and titrant must have a known, fixed ratio (e.g., 1:1).
- Equivalence Point (化学计量点): The theoretical point where the reaction is complete.
- End Point (终点): The point where we see a change (e.g., indicator colour change). Ideally, End Point $\approx$ Equivalence Point.
Types of Titrations
1. Acid-Base Titration (Aqueous) - 酸碱滴定(水相)
- Concept: Neutralisation reaction ($H^+ + OH^- \rightarrow H_2O$).
- Indicators: Weak acids or bases that change colour depending on pH (Henerson-Hasselbalch equation).
- Phenolphthalein: Colourless (Acid) $\rightarrow$ Pink (Base). Range pH 8-10.
- Methyl Orange: Red (Acid) $\rightarrow$ Yellow (Base). Range pH 3-4.5.
- Application: Strong acid/base drugs (e.g., Aspirin assay - back titration).
2. Non-Aqueous Titration (Non-Aqueous) - 非水滴定
- Why use it? Many drugs are weak bases (amines) or weak acids that do not dissociate well in water, making the endpoint sharp impossible to see. Water acts as a competing base.
- Principle: Use a solvent that enhances the acidic/basic strength of the analyte.
- Solvent: Glacial Acetic Acid (冰醋酸) is commonly used for weak bases. It removes water and acts as a protogenic solvent.
- Titrant: Perchloric Acid ($HClO_4$) in acetic acid (Strongest acid in non-aqueous media).
- Indicator: Crystal Violet.
- Clinical Example: Assay of Adrenaline, Morphine, Codeine (Weak bases).
3. Oxidation-Reduction (Redox) Titration - 氧化还原滴定
- Concept: Electron transfer.
- Titrants: Iodine ($I_2$), Permanganate ($KMnO_4$), Cerium ($Ce^{4+}$).
- Iodometry (碘量法): Indirect titration. Excess iodide ($I^-$) is added to an oxidising agent, releasing Iodine ($I_2$), which is then titrated with Thiosulfate.
- Indicator: Starch (Blue-Black $\rightarrow$ Colourless).
4. Complexometric Titration - 配位滴定
- Concept: Metal ion + Ligand $\rightarrow$ Complex.
- Reagent: EDTA (Ethylenediaminetetraacetic acid). It forms stable 1:1 complexes with most metal ions.
- Application: Analysis of Calcium, Magnesium, Zinc (e.g., Calcium Carbonate supplements).
- Indicator: Mordant Black 11 (Eriochrome Black T).
5. Calculations: Back Titration (反滴定)
Used when the reaction is slow, or the sample is insoluble (e.g., Aspirin/Acetylsalicylic Acid).
Steps:
- Add a known excess of reagent (e.g., excess NaOH to Aspirin).
- Allow the reaction to complete (hydrolysis of Aspirin).
- Titrate the remaining unreacted NaOH with acid (HCl).
- Calculation:
- Total NaOH added - Unreacted NaOH = NaOH reacted with Drug.
- Use stoichiometry to find the amount of Drug.
Summary Checklist (复习清单)
| Method | Key Reagent/Condition | Target Drugs |
|---|---|---|
| Aqueous Acid-Base | NaOH / HCl | Strong acids/bases |
| Non-Aqueous | $HClO_4$ in Acetic Acid | Weak bases (Adrenaline, Morphine) |
| Redox | Iodine / Thiosulfate | Oxidisable/Reducible drugs |
| Complexometric | EDTA | Metal ions ($Ca^{2+}, Mg^{2+}$) |
- [ ] Difference between QA and QC: Prevention vs. Detection.
- [ ] Why Non-Aqueous? Because water competes with weak bases; removing it sharpens the endpoint.
- [ ] ICH Q2: Stands for Analytical Validation.
LECTURE28 01 Core Concept 25 Pharmaceutical analysis 2
Core Concept: The interaction between electromagnetic radiation (light) and matter (drugs) provides information about the drug’s structure and concentration.
1. Introduction to Spectroscopy (光谱学简介)
The Electromagnetic Spectrum
- Energy Relationship: Energy is inversely proportional to wavelength ($\lambda$).
- High Energy = Short Wavelength (e.g., X-rays).
- Low Energy = Long Wavelength (e.g., Radio waves).
- Formula: $E = h \nu = \frac{hc}{\lambda}$ ($h$=Planck’s constant).
Major Techniques in Pharmacy
- UV-Visible (UV-Vis): Electronic transitions (valence electrons jump to higher orbitals). Used for Quantification.
- Infrared (IR): Molecular vibrations (bond stretching/bending). Used for Identification (fingerprinting).
- NMR: Nuclear spin transitions. Used for Structural Elucidation.
- Mass Spectrometry (MS): Fragmentation of molecules. Used for Molecular Weight & Structure.
2. UV-Visible Spectroscopy (紫外-可见分光光度法)
Principles (原理)
- Range:
- UV: 200 – 400 nm (Deuterium lamp source).
- Visible: 400 – 800 nm (Tungsten lamp source).
- Mechanism: Absorption of light causes electrons to move from a Ground State (Low energy) to an Excited State (High energy).
- Chromophore (发色团): The part of the molecule responsible for light absorption (usually conjugated double bonds, aromatic rings).
- Examples: Benzene rings, Carbonyl groups ($C=O$), Nitro groups ($NO_2$).
- Auxochrome (助色团): Groups that don’t absorb light themselves but shift the absorption of the chromophore (e.g., $-OH, -NH_2$).
- Bathochromic Shift (Red Shift): Shift to longer $\lambda$ (lower energy).
- Hypsochromic Shift (Blue Shift): Shift to shorter $\lambda$.
Electronic Transitions
Only certain jumps are allowed:
- $\sigma \to \sigma^*$: High energy (Vacuum UV <150nm). Not useful for standard analysis (e.g., C-H bonds).
- $n \to \pi^*$: Non-bonding electrons to anti-bonding $\pi$. Lower energy, visible in UV range (e.g., Carbonyls).
- $\pi \to \pi^*$: Bonding $\pi$ to anti-bonding $\pi$. Very useful, strong absorption (e.g., Alkenes, Aromatics).
3. The Beer-Lambert Law (比尔-朗伯定律)
The fundamental law for quantitative analysis. It states that Absorbance is directly proportional to concentration and path length.
The Equation
$$A = \log_{10} \left( \frac{I_0}{I} \right) = \epsilon \cdot c \cdot l$$
- $A$: Absorbance (No units). Note: Formerly called Optical Density (OD).
- $I_0$: Intensity of incident light.
- $I$: Intensity of transmitted light.
- $l$: Path length (usually 1 cm).
- $c$: Concentration (Molar, $mol/L$).
- $\epsilon$: Molar Absorptivity (or Molar Extinction Coefficient). Units: $L \cdot mol^{-1} \cdot cm^{-1}$. Constant for a specific drug at a specific $\lambda$.
The “A-one-one” $A(1%, 1cm)$
In the British Pharmacopoeia (BP), concentration is often expressed in % w/v (g/100ml) rather than Molar.
$$A = A(1%, 1cm) \times c \times l$$
- $c$: Concentration in % w/v.
- $A(1%, 1cm)$: Specific Absorbance. The absorbance of a 1% solution in a 1 cm cell.
Limitations of Beer’s Law (Deviations)
The linear relationship ($A \propto c$) breaks down if:
- Concentration is too high: Molecules interact with each other (Real limit: $A$ should be < 1.0 or 1.5).
- Polychromatic Light: The law assumes monochromatic light (single wavelength).
- Stray Light: Light bypassing the sample hits the detector.
- Chemical changes: pH shifts, association/dissociation, fluorescence.
4. Instrumentation (仪器)
Key Components
- Light Source: Deuterium ($D_2$) for UV; Tungsten filament for Visible.
- Monochromator: Prism or Diffraction Grating. Selects the specific wavelength ($\lambda_{max}$).
- Sample Cell (Cuvette):
- Quartz: Essential for UV (<350nm) as glass absorbs UV.
- Glass/Plastic: Okay for Visible (>350nm).
- Detector: Photomultiplier Tube (PMT) or Photodiode Array (PDA).
Single Beam vs. Double Beam
- Single Beam: Must run a “Blank” (solvent only) first to zero the machine, then run sample. Slower.
- Double Beam: Light splits. One beam goes through Reference (Blank), one through Sample. The machine automatically subtracts the blank in real-time. Corrects for light source fluctuations.
5. Fluorescence Spectroscopy (荧光光谱法)
A more sensitive technique than UV-Vis.
Mechanism (Jablonski Diagram)
- Excitation: Molecule absorbs photon, electron jumps to high energy state ($S_0 \to S_1$). (Fast: $10^{-15} s$)
- Internal Conversion: Electron loses some energy as heat (vibrational relaxation) dropping to the lowest level of $S_1$.
- Emission (Fluorescence): Electron falls back to Ground State ($S_0$) emitting a photon.
- Stokes Shift: The emitted light always has a longer wavelength (lower energy) than the absorbed light because some energy was lost as heat.
- $\lambda_{emission} > \lambda_{excitation}$
Comparison: UV vs. Fluorescence
| Feature | UV-Vis Absorption | Fluorescence Emission |
|---|---|---|
| Measurement | Difference in light intensity ($I_0$ vs $I$) | Absolute light emitted against dark background |
| Sensitivity | Moderate ($10^{-5} M$) | High ($10^{-9} M$ - Nanomolar) |
| Selectivity | Low (Many things absorb UV) | High (Fewer things fluoresce) |
| Linearity | Good at moderate conc. | Only at very low conc. |
| Structure | Conjugated systems | Rigid, planar, conjugated systems |
Quenching (猝灭)
A reduction in fluorescence intensity.
- Collisional Quenching: Excited molecule hits a quencher (e.g., Oxygen, Halides) and loses energy without emitting light.
- Concentration Quenching (Self-quenching): At high concentrations, molecules re-absorb emitted light.
6. Applications (应用)
- Quantitative Assay: Determining concentration of drugs in formulations (e.g., Paracetamol tablets).
- pKa Determination: Absorbance often changes with pH (e.g., Phenol shifts $\lambda_{max}$ when ionized).
- Dissolution Testing: Continuous monitoring of drug release from tablets.
- Impurity Testing: Detecting impurities that have different absorption spectra.
Summary Checklist (复习清单)
- [ ] Beer-Lambert Law: Can you calculate Concentration if given Absorbance and $A(1%, 1cm)$?
- Formula: $c (% w/v) = \frac{Absorbance}{A(1%, 1cm)}$
- [ ] Quartz vs Glass: Why use Quartz for UV? (Glass absorbs UV light).
- [ ] Stokes Shift: Why is emission wavelength always longer? (Energy loss due to vibrational relaxation).
- [ ] Bathochromic Shift: Red shift (to longer wavelength).
Core Concept - Oncology
LECTURE15 01 Core Concept 13 Cancer and immune disease
Core Concept: Cancer is a genetic disease of uncontrolled cell growth. The immune system can recognize and destroy cancer cells, but tumors evolve mechanisms to escape this surveillance. Immunotherapy aims to restore this anti-tumor immunity.
1. What is Cancer? (什么是癌症)
- Definition: A group of diseases characterized by the uncontrolled growth and spread of abnormal cells. It is fundamentally a genetic disease caused by mutations in DNA.
- Benign vs. Malignant (良性与恶性):
- Benign: Localized, does not invade surrounding tissue or metastasize.
- Malignant: Invades surrounding tissues and can spread (metastasize) to distant organs via blood or lymph.
- Carcinogenesis (致癌过程): A multi-step process involving the accumulation of mutations in:
- Oncogenes (原癌基因): “Accelerators” (e.g., RAS, MYC). Mutations lead to gain of function $\rightarrow$ uncontrolled division.
- Tumour Suppressor Genes (抑癌基因): “Brakes” (e.g., p53, RB). Mutations lead to loss of function $\rightarrow$ inability to stop division or repair DNA.
The Hallmarks of Cancer (癌症的特征 - Hanahan & Weinberg)
- Sustaining Proliferative Signaling: Cells grow without external signals.
- Evading Growth Suppressors: Ignoring “stop” signals (e.g., contact inhibition).
- Resisting Cell Death: Avoiding Apoptosis (programmed cell death).
- Enabling Replicative Immortality: Extending telomeres (Telomerase activation).
- Inducing Angiogenesis: Creating new blood vessels to supply oxygen/nutrients.
- Activating Invasion and Metastasis: Spreading to other parts of the body.
- Emerging Hallmarks: Deregulating cellular energetics (Warburg effect), Avoiding immune destruction.
2. Tumour Immunology (肿瘤免疫学)
The Immune Surveillance Theory (免疫监视理论)
The immune system constantly identifies and eliminates pre-cancerous cells. However, cancer cells are “Self” cells, making them harder to target than bacteria.
Tumour Antigens (肿瘤抗原)
How does the immune system see cancer?
- Tumour-Specific Antigens (TSAs): Unique to cancer cells (e.g., mutated p53 products, viral antigens like HPV). Ideal targets.
- Tumour-Associated Antigens (TAAs): Normal proteins expressed at abnormally high levels or in wrong tissues (e.g., HER2, CEA).
Cancer Immunoediting: The “3 Es” (癌症免疫编辑)
The dynamic process between the tumour and immune system:
- Elimination (清除): Innate and adaptive immunity (NK cells, CD8+ T cells) detect and destroy cancer cells.
- Equilibrium (平衡): Some cancer cells survive but are kept in check. They undergo genetic instability and selection.
- Escape (逃逸): Tumour cells evolve mechanisms to suppress the immune system or hide from it, leading to clinical disease.
Mechanisms of Immune Escape (免疫逃逸机制)
- Downregulation of MHC Class I: “Hiding” from CD8+ T cells.
- Expression of Inhibitory Ligands: e.g., PD-L1 on tumour surface binds to PD-1 on T cells to turn them off.
- Recruitment of Suppressive Cells: Tregs (Regulatory T cells), MDSCs (Myeloid-derived suppressor cells) which secrete immunosuppressive cytokines (IL-10, TGF-$\beta$).
3. Cancer Immunotherapy (癌症免疫疗法)
Goal: To “release the brakes” on the immune system or engineer it to attack cancer.
A. Immune Checkpoint Inhibitors (免疫检查点抑制剂)
Checkpoints are normal “off switches” to prevent autoimmunity. Cancers hijack them.
| Checkpoint | Mechanism | Drug Examples (Monoclonal Antibodies) |
|---|---|---|
| CTLA-4 | Operates in Lymph Nodes. Prevents T-cell activation (priming phase). | Ipilimumab (Yervoy) |
| PD-1 | Operates in Peripheral Tissue (Tumour). Receptor on T-cells. “Exhaustion” signal. | Nivolumab (Opdivo), Pembrolizumab (Keytruda) |
| PD-L1 | Ligand on Tumour Cells. Binds to PD-1 to shut down T-cell. | Atezolizumab (Tecentriq), Durvalumab |
- Clinical Success: remarkably effective in Melanoma, Lung Cancer (NSCLC), Renal Cancer.
- Side Effects: Immune-Related Adverse Events (irAEs).
- The immune system attacks normal tissue: Colitis (diarrhoea), Pneumonitis (lung inflammation), Dermatitis (rash), Hepatitis, Thyroiditis.
- Management: High-dose Corticosteroids (to suppress the overactive immune system).
B. CAR-T Cell Therapy (嵌合抗原受体T细胞疗法)
“Living Drug” - Engineering the patient’s own cells.
- Collection: T cells are harvested from the patient (Leukapheresis).
- Engineering: Genetically modified ex vivo to express a Chimeric Antigen Receptor (CAR).
- The CAR: Fuses an antibody fragment (recognizes cancer directly, independent of MHC) with T-cell signaling domains.
- Expansion: Grown in the lab to billions.
- Infusion: Infused back into the patient.
- Target: Usually CD19 (found on B-cell Leukemias and Lymphomas).
- Toxicities:
- Cytokine Release Syndrome (CRS): “Cytokine Storm” (Fever, Hypotension). Treated with Tocilizumab (Anti-IL-6).
- Neurotoxicity (ICANS): Confusion, seizures.
C. Other Modalities
- Cancer Vaccines: Therapeutic (e.g., Provenge for prostate) or Prophylactic (e.g., HPV vaccine).
- Bi-specific T-cell Engagers (BiTEs): Antibodies with two arms—one grabs the cancer cell, one grabs the T cell, forcing them together (e.g., Blinatumomab).
4. Summary: Traditional vs. Immuno-Oncology
| Feature | Chemotherapy | Targeted Therapy | Immunotherapy |
|---|---|---|---|
| Target | Rapidly dividing cells (DNA/Microtubules) | Specific Mutations (e.g., EGFR, BRAF) | The Patient’s Immune System |
| Specificity | Low (Kills hair, gut cells too) | High | Variable (Depends on antigen) |
| Duration | Effect stops when drug stops | Resistance often develops quickly | Durable Memory (Potential for long-term cure) |
| Side Effects | Nausea, Hair loss, Neutropenia | Specific to target | Autoimmune-like (irAEs) |
LECTURE36 01 Core Concept 32 Introduction to SACT Toxicities
Core Focus: Understanding the side effects of Systemic Anti-Cancer Therapy (SACT), grading severity, and managing oncological emergencies.
1. What is SACT? (什么是全身抗癌治疗)
SACT (Systemic Anti-Cancer Therapy) is an umbrella term that includes:
- Cytotoxic Chemotherapy (细胞毒性化疗): Traditional drugs that kill rapidly dividing cells.
- Immunotherapy (免疫疗法): Checkpoint inhibitors (e.g., Nivolumab).
- Targeted Therapy (靶向治疗): Monoclonal antibodies (e.g., Trastuzumab) or Small molecules (e.g., Imatinib).
- Hormonal Therapy (激素疗法): e.g., Tamoxifen.
The “Why” of Toxicity:
Cytotoxic drugs targets rapidly dividing cells (快速分裂的细胞). They cannot distinguish between cancer cells and healthy cells with high turnover rates, such as:
- Bone Marrow (骨髓): Leads to myelosuppression (infection, anaemia, bleeding).
- Gastrointestinal Tract (胃肠道): Leads to mucositis, diarrhoea, nausea.
- Hair Follicles (毛囊): Leads to alopecia (hair loss).
2. Grading of Toxicity: CTCAE (毒性分级)
We use the Common Terminology Criteria for Adverse Events (CTCAE - 不良事件通用术语标准) to standardize reporting.
| Grade (分级) | Severity (严重程度) | Clinical Description (临床描述) |
|---|---|---|
| Grade 1 | Mild (轻度) | Asymptomatic or mild symptoms; observation only. |
| Grade 2 | Moderate (中度) | Minimal, local or non-invasive intervention indicated. |
| Grade 3 | Severe (重度) | Medically significant but not immediately life-threatening; hospitalization indicated. |
| Grade 4 | Life-threatening (危及生命) | Urgent intervention indicated. |
| Grade 5 | Death (死亡) | Death related to AE. |
3. Bone Marrow Suppression (骨髓抑制 - Myelosuppression)
The most common dose-limiting toxicity. It affects three cell lines:
- Neutropenia (中性粒细胞减少): Risk of life-threatening infection.
- Anaemia (贫血): Fatigue, breathlessness. Treated with blood transfusion or EPO.
- Thrombocytopenia (血小板减少): Risk of bleeding. Treated with platelet transfusion.
Neutropenic Sepsis (中性粒细胞减少性败血症) - MEDICAL EMERGENCY
This is the single most critical concept in this lecture.
-
Definition (定义):
- Neutrophil count < 0.5 x 10^9/L (Severe Neutropenia)
- AND
- Temperature > 38°C OR other signs of sepsis (hypotension, tachycardia).
-
Pathophysiology:
- Chemotherapy destroys neutrophils (immune soldiers).
- Patient cannot mount an immune response (no pus, no inflammation).
- Fever may be the only sign of severe infection.
- Death can occur within hours if untreated.
-
Management: “Door to Needle” < 1 Hour (进门到给药小于1小时):
- Do NOT wait for blood results if suspected. Treat empirically immediately.
- First-line Antibiotics: usually Piperacillin/Tazobactam (Tazocin) (Broad spectrum IV antibiotic).
- Often combined with Gentamicin.
-
Risk Stratification: MASCC Score (MASCC 评分):
- Used to assess the risk of complications in febrile neutropenia.
- High Score (> 21): LOW Risk. (Confusing, but remember: High score is Good). May be treated with oral antibiotics at home.
- Low Score (< 21): HIGH Risk. Requires aggressive IV therapy in hospital.
4. Gastrointestinal Toxicities (胃肠道毒性)
A. Nausea & Vomiting (CINV - 化疗诱导的恶心呕吐)
Classified into three types:
- Acute (急性): Occurs within 24 hours. Mediated by Serotonin (5-HT3).
- Treatment: 5-HT3 Antagonists (Ondansetron) + Dexamethasone.
- Delayed (迟发性): Occurs after 24 hours (days 2-5). Mediated by Substance P (Neurokinin-1).
- Treatment: NK1 Antagonists (Aprepitant) + Dexamethasone + Metoclopramide.
- Anticipatory (预期性): Psychological conditioned response (vomiting before chemo).
- Treatment: Benzodiazepines (Lorazepam) and behavioral therapy.
Emetogenicity (致吐性分级): Drugs are classified by risk (High, Moderate, Low, Minimal). E.g., Cisplatin is High Risk (>90% vomiting without prophylaxis).
B. Mucositis (粘膜炎)
- Inflammation and ulceration of the GIT lining (mouth to anus).
- Oral Mucositis: Very painful ulcers, prevents eating/drinking.
- Management: Pain relief (Difflam mouthwash, Morphine), Oral hygiene, Ice chips (Cryotherapy).
5. Other Specific Toxicities (其他特定毒性)
A. Alopecia (脱发)
- Common with Taxanes (Docetaxel) and Anthracyclines (Doxorubicin).
- Scalp Cooling (头皮冷却/冰帽): Constricts blood vessels in the scalp $\rightarrow$ less drug reaches hair follicles $\rightarrow$ reduces hair loss.
B. Extravasation (外渗)
- Definition: Leakage of chemotherapy drug from the vein into surrounding tissue.
- Vesicants (起疱剂): Cause severe tissue necrosis (skin death) and permanent damage. e.g., Anthracyclines (Doxorubicin), Vinca Alkaloids (Vincristine).
- Irritants (刺激剂): Cause inflammation/pain but no necrosis.
- Management: STOP infusion immediately. Leave cannula in to aspirate drug. Apply Hot or Cold pack (depends on drug). Use antidotes (e.g., Hyaluronidase for Vinca Alkaloids).
C. Infertility (不孕不育)
- Chemotherapy can damage sperm/eggs.
- Advice: Sperm banking (men) or Embryo freezing (women) before starting treatment.
D. Immunotherapy Side Effects (irAEs - 免疫相关不良事件)
- Checkpoint inhibitors “take the brakes off” the immune system.
- Result: The immune system attacks the body (Autoimmunity).
- Symptoms: Anything ending in “-itis” (Colitis, Pneumonitis, Hepatitis, Thyroiditis).
- Treatment: Stop drug + High dose Steroids (to suppress immunity).
Summary Checklist (复习清单)
- [ ] Neutropenic Sepsis: Neutrophils < 0.5 + Fever. Treatment: IV Antibiotics within 1 hour.
- [ ] MASCC Score: Score > 21 = Low Risk (Good). Score < 21 = High Risk (Bad).
- [ ] CINV Mechanisms: Acute = 5-HT3 (Serotonin); Delayed = NK1 (Substance P).
- [ ] Vesicants: Drugs that cause necrosis if extravasated (e.g., Doxorubicin, Vincristine).
- [ ] CTCAE: The standard scale for grading toxicity (Grade 1-5).
LECTURE37 01 Core Concept 33 Lung cancer initiation and demographics
Lecturer: Professor Kaye Williams
Core Concept: Understanding why lung cancer is the leading cause of cancer death, how genetic mutations drive initiation, and the mechanistic link with COPD.
1. Overview of Cancer
- Definition: Cancer is caused by “out of control” cell growth that can affect any cell type.
- The Hallmarks of Cancer (癌症的特征 - Hanahan & Weinberg):
Tumours are complex tissues, not just bags of mutant cells. Key capabilities include:- Sustaining Proliferative Signaling (持续增殖信号): Growing without external instructions.
- Evading Growth Suppressors (逃避生长抑制): Ignoring “stop” signals.
- Resisting Cell Death (抵抗细胞死亡): Avoiding Apoptosis (程序性死亡).
- Enabling Replicative Immortality (无限复制能力): Extending telomeres.
- Inducing Angiogenesis (诱导血管生成): Creating new blood vessels for oxygen/nutrients.
- Activating Invasion and Metastasis (激活侵袭和转移): Spreading to other organs.
- Emerging: Deregulating Cellular Energetics (Warburg effect - altered metabolism).
- Emerging: Avoiding Immune Destruction (Hiding from T-cells).
2. Lung Cancer Demographics (肺癌人口统计学)
Incidence vs. Mortality (发病率与死亡率)
- Incidence: It is the 3rd most common cancer in the UK (after Breast and Prostate).
- Mortality: It is the Number 1 cause of cancer death in the UK.
- Reason: It is often diagnosed at a late stage (Stage 3 or 4) because symptoms (cough) are non-specific and ignored.
- Survival: 10-year survival is remarkably low (~5-10%) compared to Breast/Prostate (~80%+).
Risk Factors (风险因素)
- Smoking (吸烟): The dominant factor (linked to ~85% of cases).
- However, not all smokers get lung cancer (only ~10-15%), and not all lung cancer patients are smokers. This suggests underlying Genetic Susceptibility (遗传易感性).
- Age (年龄): Incidence peaks at 75–84 years. It is a disease of ageing (accumulation of mutations over time).
- Deprivation (贫困/社会剥夺):
- Incidence is much higher in deprived areas.
- Link: largely driven by higher smoking rates in these populations.
- Sex (性别): Historically higher in men, but the gap is narrowing as female smoking rates changed in the late 20th century.
3. Cancer Initiation: Genetics
Cancer is a genetic disease caused by the accumulation of mutations in three key gene classes:
A. Oncogenes (原癌基因)
- Function: Normally promote cell growth/division (Proto-oncogenes).
- Mutation Effect: Gain of Function (功能获得). Like an “Accelerator” stuck down.
- Inheritance: Dominant (显性). Only one mutated allele is needed to trigger uncontrolled growth.
- Examples: KRAS, EGFR, MYC.
B. Tumour Suppressor Genes (TSGs - 抑癌基因)
- Function: Normally inhibit cell division or repair DNA (“The Brakes”).
- Mutation Effect: Loss of Function (功能缺失). Like “Brakes” failing.
- Inheritance: Recessive (隐性). Two mutated alleles are needed (both copies must be broken).
- Knudson’s Two-Hit Hypothesis (二次打击假说):
- Hit 1: You might inherit one bad copy (germline) OR acquire it (somatic). Cell is still normal because the other copy works.
- Hit 2: The second copy mutates. Now the cell becomes cancerous.
- Examples: p53 (Guardian of the genome), RB (Retinoblastoma).
C. DNA Repair Genes (DNA修复基因)
- Function: Fix errors during DNA replication.
- Mutation: Leads to Genomic Instability (基因组不稳定性), accelerating the mutation rate in other genes.
- Example: BRCA1/2.
4. The Link: COPD and Lung Cancer (COPD与肺癌的联系)
Patients with COPD have a significantly higher risk of developing lung cancer (up to 4-5x), even when adjusting for smoking. Why?
Shared Mechanisms (共同机制)
- Chronic Inflammation (慢性炎症):
- Inflammatory cells (Neutrophils, Macrophages) release ROS (Reactive Oxygen Species - 活性氧) which damage DNA.
- They release cytokines that promote cell proliferation and angiogenesis.
- Epithelial-Mesenchymal Transition (EMT - 上皮-间质转化):
- Cells lose their sticky structure and become mobile (fibrous), aiding metastasis.
- Field Cancerization (区域癌化):
- Concept: Smoking doesn’t just damage one spot; it bathes the entire airway in carcinogens.
- Large areas of tissue contain pre-cancerous mutations (mutant clones), even if they look normal microscopically.
- Result: You might surgically remove a tumour, but the remaining “normal” tissue is already primed to spawn a new tumour (Second Primary Tumour).
5. Clinical Presentation: Red Flags
Pharmacists play a key role in early detection by spotting these symptoms in patients buying cough medicines repeatedly.
- Persistent Cough (持续咳嗽): Lasting > 3 weeks (Unexplained).
- Haemoptysis (咯血): Coughing up blood (Major red flag).
- Recurrent Chest Infections (反复胸部感染): Antibiotics don’t clear it, or it keeps coming back.
- Breathlessness (呼吸困难): Worsening dyspnoea.
- Systemic Symptoms (全身症状):
- Weight Loss (体重减轻): Unexplained.
- Fatigue (疲劳): Cancer cells hijack energy (Warburg effect) and cause hypoxia.
- Loss of Appetite (食欲不振).
Clinical Pearl: If a patient aged 40+ (especially a smoker) comes to the pharmacy with a cough lasting >3 weeks or is repeatedly buying cough syrup, REFER them for a Chest X-ray/GP appointment. Early diagnosis saves lives.
LECTURE39 01 Core Concept 35 Cancer hallmarks to targeted therapies
Lecturer: Professor Kaye Williams
Core Concept: Moving from cytotoxic chemotherapy to molecularly targeted agents based on the specific genetic profile of the tumour.
1. The Shift in Treatment Paradigm (治疗范式的转变)
Standard Chemotherapy (标准化疗)
- Mechanism: Targets rapidly dividing cells (nonspecific).
- Limitations (局限性):
- Lack of Selectivity (缺乏选择性): Kills healthy rapidly dividing cells (hair follicles, gut lining, bone marrow).
- Side Effects: Alopecia (脱发), Nausea/Vomiting (恶心呕吐), Neutropenia (中性粒细胞减少/免疫力低下).
- Efficacy: Often has a “ceiling” effect; not curative for advanced metastatic disease.
Targeted Therapy (靶向治疗)
- Mechanism: Targets specific molecular deregulations (proteins/genes) driving the cancer.
- Goal: High selectivity for tumour cells, reduced systemic toxicity, improved Quality of Life (QoL).
- Key Requirement: Requires Precision Medicine (精准医疗) — knowing the specific genetic makeup of the patient’s tumour before prescribing.
2. Targeting the Hallmarks of Cancer (靶向癌症特征)
Based on Hanahan & Weinberg’s “Hallmarks of Cancer”.
- Sustaining Proliferative Signaling (持续增殖信号):
- Cancer cells constitutively activate growth pathways.
- Key Target: Receptor Tyrosine Kinases (RTKs - 受体酪氨酸激酶).
- Mechanism: Ligand binds $\rightarrow$ Dimerization $\rightarrow$ Autophosphorylation $\rightarrow$ Downstream signalling (RAS/RAF/MEK or PI3K/AKT) $\rightarrow$ Cell Proliferation/Survival.
- Drug Class: Tyrosine Kinase Inhibitors (TKIs - 酪氨酸激酶抑制剂). Small molecules that block the ATP binding site of the kinase, preventing phosphorylation.
3. Key Targets in Lung Cancer (NSCLC) (非小细胞肺癌的关键靶点)
Lung cancer is the “poster child” for targeted therapy. Pharmacists must know these specific mutations and drugs.
A. EGFR (Epidermal Growth Factor Receptor - 表皮生长因子受体)
- Prevalence: Common in Never-smokers, Females, and Asian ethnicity (up to 50% in Asian populations).
- Driver Mutations (驱动突变):
- Exon 19 Deletion (Exon 19 del).
- Exon 21 Point Mutation (L858R).
- Effect: These mutations make the receptor “stuck” in the ON position, constantly driving growth.
- Therapies (EGFR-TKIs):
- 1st Generation: Gefitinib, Erlotinib. (Reversible inhibitors).
- 2nd Generation: Afatinib. (Irreversible inhibitor).
- 3rd Generation: Osimertinib. (The current Gold Standard).
- Toxicities (副作用):
- Acne-form Rash (痤疮样皮疹): Mechanism-based toxicity (EGFR is abundant in skin). Management: Moisturisers, steroid creams, antibiotics (doxycycline).
- Diarrhoea (腹泻).
- Resistance (耐药性):
- After ~10-14 months, tumours develop resistance.
- T790M Mutation: The “Gatekeeper” mutation. It changes the binding pocket so 1st gen drugs can’t fit.
- Solution: Osimertinib specifically targets T790M and is also CNS-penetrant (treats brain metastasis).
B. ALK (Anaplastic Lymphoma Kinase - 间变性淋巴瘤激酶)
- Mechanism: Gene Rearrangement / Fusion (基因重排/融合).
- The EML4 gene fuses with the ALK gene. The resulting fusion protein is always active.
- Prevalence: ~3-7% of NSCLC. Younger patients, never/light smokers.
- Therapies (ALK Inhibitors):
- Crizotinib (1st Gen).
- Alectinib, Brigatinib, Lorlatinib (Next Gen - better brain penetration and cover resistance).
C. ROS1 (ROS Proto-Oncogene 1)
- Mechanism: Gene Fusion (similar to ALK).
- Therapies:
- Crizotinib (Originally for ALK, but ROS1 is structurally similar).
- Entrectinib.
D. KRAS G12C (Kirsten Rat Sarcoma Viral Oncogene)
- History: Considered “Undruggable” for decades because the protein is a smooth sphere with no obvious binding pockets.
- Breakthrough: Scientists found a small “switch II pocket” that only exists in the mutant form (G12C).
- Drug: Sotorasib (Lumykras).
- Indication: For patients who have failed chemotherapy and have the specific G12C mutation (Glycine to Cysteine at position 12).
- Significance: A major milestone in targeting the most common oncogene in human cancer.
4. Companion Diagnostics (伴随诊断)
You cannot treat what you do not test.
- Definition: A diagnostic test used to identify patients who are likely to benefit from a specific drug.
- Testing Methods:
- PCR / NGS (Next Generation Sequencing): To detect specific DNA mutations (EGFR, KRAS).
- FISH (Fluorescence In Situ Hybridisation): To visualize gene translocations/fusions (ALK, ROS1).
- IHC (Immunohistochemistry): To detect protein expression (PD-L1 levels).
- Role of Pharmacist: Ensure the test result is positive before verifying/dispensing the targeted drug.
Summary Table (Lung Cancer Targets)
| Target (靶点) | Type of Alteration (变异类型) | Drug Examples (药物) | Key Notes (要点) |
|---|---|---|---|
| EGFR | Mutation (Exon 19/21) | Osimertinib, Gefitinib | Common in Asian/Non-smokers. Rash is key side effect. |
| ALK | Fusion (EML4-ALK) | Alectinib, Crizotinib | Younger patients. |
| ROS1 | Fusion | Crizotinib, Entrectinib | Similar to ALK. |
| KRAS | Mutation (G12C) | Sotorasib | Previously “undruggable”. |
| NTRK | Fusion | Larotrectinib | “Tumour Agnostic” (works in any cancer with this fusion). |
LECTURE40 01 Core Concept 36 Inflammation cancer biology to targeted therapies
Lecturer: Professor Kaye Williams
Core Concept: The immune system has a “dual role” in cancer. It can suppress tumour growth (Immune Surveillance), but chronic inflammation can promote tumour initiation and progression. Immunotherapy aims to restore the anti-tumour function.
1. Inflammation and Cancer Initiation (炎症与癌症的发生)
Chronic inflammation is a key driver of cancer risk (e.g., COPD $\rightarrow$ Lung Cancer; Hepatitis $\rightarrow$ Liver Cancer).
Mechanisms of Initiation
- Genomic Instability (基因组不稳定性):
- Inflammatory cells (Neutrophils/Macrophages) release Reactive Oxygen Species (ROS - 活性氧) and Reactive Nitrogen Species.
- These cause DNA damage and mutations.
- The “Two-Hit” Hypothesis (二次打击假说):
- Scenario A: Single Mutation + No Inflammation $\rightarrow$ No Tumour (Cell undergoes apoptosis or repair).
- Scenario B: Inflammation + No Mutation $\rightarrow$ No Tumour (Tissue heals).
- Scenario C (The Danger Zone): Inflammation + Single Mutation $\rightarrow$ Tumour.
- Explanation: Inflammation acts as a Tumour Promoter (肿瘤促进剂). It stimulates the mutated cell to proliferate rather than die, allowing the mutation to become “fixed” in the population.
2. The Tumour Microenvironment (TME - 肿瘤微环境)
A tumour is not just a ball of cancer cells. It is a complex organ containing:
- Cancer Cells.
- Stromal Cells: Fibroblasts, Endothelial cells (blood vessels).
- Immune Cells (Infiltrate): Macrophages, T-cells, Neutrophils.
“Reprogramming” the Immune System (免疫系统的“重编程”)
Cancer cells manipulate the immune cells in the TME to switch from “Attack Mode” to “Help Mode”.
- Pro-tumourigenic Inflammation (促肿瘤炎症):
- Immune cells release Growth Factors (promote proliferation).
- Release Angiogenic Factors (VEGF) $\rightarrow$ New blood vessels.
- Release enzymes (Matrix Metalloproteinases - MMPs) that break down tissue $\rightarrow$ Aid Metastasis (转移).
3. Immune Surveillance vs. Evasion (免疫监视与逃逸)
Immune Surveillance (免疫监视)
Normally, CD8+ Cytotoxic T-cells (细胞毒性T细胞) recognise abnormal antigens on cancer cells and kill them.
Mechanisms of Immune Evasion (免疫逃逸机制)
How does the tumour survive?
- Downregulation of MHC Class I: The tumour stops presenting antigens (“Hiding”).
- T-cell Exhaustion (T细胞耗竭): T-cells are present but inactive.
- Expression of Immune Checkpoints (免疫检查点): The most critical mechanism for therapy.
4. The PD-1 / PD-L1 Pathway (PD-1 / PD-L1 通路)
This is the target of modern immunotherapy in Lung Cancer.
- PD-1 (Programmed Cell Death Protein 1): A receptor on the surface of T-cells. It acts as an “Off Switch” or “Brake” to prevent autoimmunity.
- PD-L1 (Programmed Cell Death Ligand 1): The ligand that binds to PD-1.
- Normal Function: Healthy tissues express PD-L1 to tell T-cells “Don’t attack me.”
- Cancer Hijack: Tumour cells express high levels of PD-L1.
- The Interaction:
- Tumour PD-L1 binds to T-cell PD-1.
- Result: The T-cell is deactivated (anergy/exhaustion) and cannot kill the cancer cell.
5. Targeted Therapies: Checkpoint Inhibitors (免疫检查点抑制剂)
Mechanism of Action (MOA):
These are Monoclonal Antibodies (单克隆抗体) that block the interaction between PD-1 and PD-L1. This “releases the brakes” on the T-cells, allowing them to attack the tumour.
Key Drugs in Lung Cancer (NSCLC)
- Anti-PD-1 Antibodies (Target the T-cell):
- Pembrolizumab (Keytruda)
- Nivolumab (Opdivo)
- Anti-PD-L1 Antibodies (Target the Tumour):
- Durvalumab (Imfinzi)
- Atezolizumab (Tecentriq)
Clinical Evidence: The PACIFIC Trial (PACIFIC 临床试验)
- Context: Stage III NSCLC (Locally advanced, unresectable).
- Protocol: Patients received Standard Chemotherapy + Radiotherapy (ChemoRT).
- Intervention: Followed by maintenance therapy with Durvalumab (Anti-PD-L1).
- Result: Significantly improved Progression-Free Survival (PFS) and Overall Survival compared to placebo.
- Mechanism Note: Chemotherapy and Radiotherapy can actually upregulate PD-L1 on dying tumour cells, making the subsequent immunotherapy even more effective (Synergy).
Summary of Strategy (治疗策略总结)
- Test: Check PD-L1 expression levels (using Immunohistochemistry - IHC) on the biopsy. High expression usually correlates with better response.
- Treat: Use Checkpoint Inhibitors alone or in combination with Chemotherapy.
- Side Effects (irAEs): Because we release the brakes on the immune system, the patient may develop autoimmune conditions (Pneumonitis, Colitis, etc.).
Summary Table (Target vs. Therapy)
| Target (靶点) | Role (作用) | Drug Class (药物类别) | Example Drugs (代表药物) |
|---|---|---|---|
| EGFR / ALK / KRAS | Driver Mutations (Oncogenes) | Tyrosine Kinase Inhibitors (TKI) | Osimertinib, Sotorasib |
| PD-1 | T-cell “Off Switch” | Checkpoint Inhibitor (Antibody) | Pembrolizumab, Nivolumab |
| PD-L1 | Tumour Shield (Ligand) | Checkpoint Inhibitor (Antibody) | Durvalumab, Atezolizumab |
Core Concept - Professional Skills & Law
LECTURE25 01 Core Concept 22 Interactive Lecture CDs, instalments and emergency supply
Focus: Legal requirements for Schedule 2 & 3 CDs, FP10MDA forms, and Emergency Supply regulations.
1. Controlled Drug Prescriptions (管制药物处方 - Schedule 2 & 3)
Prescriptions for Schedule 2 (e.g., Morphine, Methadone) and Schedule 3 (e.g., Gabapentin, Tramadol, Midazolam) generally have stricter writing requirements than standard POMs.
A. Legal Requirements (必须满足的法律要求)
The prescriber MUST include the following on the prescription (Rx):
- Signature: Usually usually be in ink and handwritten by the prescriber (unless it’s a compliant Electronic Prescription Service - EPS).
- Date: Can be computer-generated.
- Validity (有效期):
- Schedule 2, 3 & 4: Valid for 28 days from the date on the Rx (or the start date).
- Schedule 5: Valid for 6 months (same as standard POM).
- Validity (有效期):
- Prescriber’s Address: Must be in the UK.
- Patient’s Name & Address: Must be fixed (No “No Fixed Abode” allowed generally for CDs unless specific arrangements).
- Dose (剂量): Must be clear and specific.
- “One as directed” (遵医嘱) is NOT acceptable for Sch 2 & 3. It must say e.g., “One tablet twice daily”.
- “As required” (PRN) is acceptable ONLY IF a maximum frequency/dose is stated (e.g., “One every 4-6 hours when required, max 4 per day”).
- Formulation (剂型): Must be specified (e.g., “Tablets”, “Capsules”).
- Even if only one form exists, it is good practice (and often legal necessity for clarity) to state it. Abbreviation like “Caps” is usually acceptable.
- Strength (规格): Only required if the drug comes in multiple strengths.
- Total Quantity (总量):
- MUST be written in both WORDS and FIGURES (e.g., “10 (Ten)”).
- This is to prevent tampering (e.g., adding a zero).
B. Pharmacist Amendments (药师修改权)
Pharmacists can amend minor typographical or spelling errors on Sch 2 & 3 prescriptions if the prescriber’s intention is clear.
- Can amend: Minor typos, spelling mistakes, or if the quantity is missing in either words or figures (but not both) and the intention is obvious.
- Cannot amend: The Signature or the Date. If these are missing, the Rx must be returned.
- Process: Amend in ink, sign, name, GPhC number, and date the amendment.
C. Quantity Limits (数量限制)
- Good Practice: Department of Health recommends a maximum of 30 days’ supply for CDs.
- Legal Status: This is NOT a law, it is guidance. You can dispense more if clinically justified (e.g., patient going on holiday), but you should document the reason.
2. Instalment Dispensing (分期调配)
Used primarily for the management of substance misuse (e.g., Methadone, Buprenorphine).
The FP10MDA Form (Blue Form)
- Purpose: Allows a single prescription to be dispensed to the patient in multiple “instalments” over a period (usually 14 days).
- Key Requirements:
- Amount per Instalment: Must state exactly how much to give each time (e.g., “60ml”).
- Interval: Must state when to give it (e.g., “Daily”, “Mon/Wed/Fri”).
- Supervision: Often requires “Supervised Consumption” (patient drinks it in front of the pharmacist).
The “Three Day Rule” (Missed Doses)
- If a patient on daily supervised maintenance (e.g., Methadone) misses 3 consecutive days (三天连续漏服):
- Action: DO NOT DISPENSE.
- Reason: Their tolerance may have dropped, and the usual dose could now be fatal (Overdose risk).
- Procedure: Refer the patient back to the prescriber for re-titration.
3. Emergency Supply (紧急供应)
Under the Human Medicines Regulations 2012, pharmacists can supply POMs without a prescription in an emergency.
Route A: Request by Prescriber (医生请求)
- The doctor calls and asks you to give medicine to a patient, promising to send the Rx later.
- Condition: You must be satisfied the request is genuine.
- Rx Delivery: The prescriber must furnish the prescription within 72 hours.
- CDs: You CANNOT supply Sch 1, 2, or 3 CDs on an emergency request from a prescriber (unless Phenobarbital for epilepsy).
Route B: Request by Patient (患者请求)
More common in community pharmacy (e.g., ran out of meds on weekend).
Conditions (Interview Requirements):
- Interview: You must interview the patient (usually).
- Immediate Need: There is an immediate need for the medicine.
- Impracticable: It is impracticable for the patient to obtain a prescription (e.g., GP closed).
- Previous Treatment: The medicine has been prescribed for them before.
- Dose: You know the correct dose.
Restrictions on Controlled Drugs (CDs):
- General Rule: Emergency supply is NOT ALLOWED for Schedule 1, 2, or 3 drugs.
- Examples of banned supply: Morphine, Oxycodone, Temazepam, Gabapentin, Tramadol.
- The Exception: Phenobarbital (Sodium Phenobarbitone) for Epilepsy IS permitted.
Maximum Quantity Rules (Supply Limits):
- Schedule 4 & 5 CDs (and Phenobarbital exception): Max 5 days supply.
- Standard POMs: Max 30 days supply.
- Exceptions to the 30-day rule:
- Insulin / Creams / Inhalers: Supply the smallest pack available (cannot break packs).
- Oral Contraceptives: Supply a full cycle (e.g., 21 tablets or 3 months depending on type).
- Antibiotics (Oral): Generally should not be supplied (risk of resistance), but technically allowed if smallest pack for a full course.
Summary Cheat Sheet (复习速查表)
| Feature | Schedule 2 (e.g. Morphine) | Schedule 3 (e.g. Tramadol) | Schedule 4/5 (e.g. Diazepam) | Standard POM |
|---|---|---|---|---|
| Rx Validity | 28 Days | 28 Days | 28 Days | 6 Months |
| Total Quantity | Words & Figures | Words & Figures | Figures only (usually) | Figures only |
| Emergency Supply (Patient) | NO | NO (except Phenobarb) | Yes (Max 5 days) | Yes (Max 30 days*) |
| Repeat Rx Allowed? | No | No | Yes | Yes |
Clinical Note:
- Always check the date on a CD script first. If it’s >28 days, it is legally invalid.
- If a doctor forgets to write the quantity in words for Morphine, you (the pharmacist) can amend it if the intention is clear, but you must sign and date the amendment.
LECTURE35 01 Core Concept 31 Interactive Law Tutorial -POMS PointSolutions
Core Focus: Legal validity of prescriptions, Emergency Supply rules, and EEA/Swiss prescriptions.
1. Prescription Validity & Legality (处方有效性与合法性)
A. General Requirements for POM (处方药的一般要求)
A legally valid prescription for a Prescription Only Medicine (POM) must include:
- Signature (签名): Must be signed in ink by the prescriber (unless it is a compliant Electronic Prescription Service - EPS).
- Address (地址): The prescriber’s address must be stated and must be in the UK (for standard UK prescriptions).
- Date (日期): Valid for 6 months from the date on the prescription.
- Note: For Controlled Drugs (CDs) Schedule 2, 3, and 4, it is valid for only 28 days.
- Patient Details (患者信息): Name and Address.
- Age (年龄): Required if the patient is under 12 years old.
B. The “Faxed Prescription” Scenario (传真处方场景)
- Scenario: A doctor faxes a prescription to the pharmacy and asks you to dispense it.
- Legal Status: A fax is NOT a legally valid prescription in the UK (it is a copy, not the original signed in ink).
- Action: You cannot dispense “against” the fax.
- Solution: You must treat this as an Emergency Supply at the request of a Prescriber (处方医师请求的紧急供应).
- You supply the medication based on the doctor’s request.
- The doctor legally must furnish the original prescription within 72 hours.
2. Emergency Supply (紧急供应)
Allows pharmacists to supply POMs without a prescription in emergencies. There are two routes:
Route A: Request by Prescriber (医师请求)
- Trigger: Doctor/Dentist calls or faxes.
- Condition: You are satisfied the request is genuine.
- Time Limit: Hard copy Rx must be received within 72 hours.
- CD Restrictions: NO Schedule 1, 2, or 3 CDs allowed (Except Phenobarbital for epilepsy).
Route B: Request by Patient (患者请求)
-
Conditions (Interview):
- Interview (面谈): Must interview the patient (unless strictly not possible).
- Immediate Need (急需): Health would suffer without it.
- Impracticable (不可行): Not feasible to get a prescription (e.g., GP closed, weekend).
- Previous Treatment (既往治疗): Prescribed by a UK/EEA prescriber previously.
- Dose: You know the correct dose.
-
Quantity Rules (供应数量规则):
- General POMs: Maximum 30 days supply.
- Exceptions (例外情况):
- Controlled Drugs (Sch 4 & 5) / Phenobarbital: Max 5 days supply.
- Insulin / Inhalers / Creams: Supply the smallest pack available (do not break packs).
- Oral Contraceptives (口服避孕药): Supply a full treatment cycle (e.g., 21 days or 3 months pack depending on brand).
- Antibiotics: Generally avoided, but if liquid for a child, supply smallest pack.
3. EEA & Swiss Prescriptions (欧洲经济区与瑞士处方)
Prescriptions from the European Economic Area (EEA) and Switzerland are legally recognized in the UK.
Who can prescribe? (谁有权开方?)
- Doctors (医生)
- Dentists (牙医)
- Pharmacists (药师 - Note: Assuming prescribing rights exist in their country)
- Nurses (护士 - Note: Assuming prescribing rights exist)
Limitations (限制)
- Controlled Drugs: CANNOT dispense Schedule 1, 2, or 3 CDs on an EEA/Swiss prescription. (Schedule 4 and 5 are permitted).
- Marketing Authorisation: The medicine must have a UK marketing authorisation (or be a generic equivalent).
- Language: Ideally in English, but legally valid if you can interpret it safely.
Emergency Supply for EEA Prescribers?
- Yes. You can make an emergency supply at the request of an EEA/Swiss prescriber, provided the 72-hour rule for the hard copy is followed.
4. Private Prescriptions & Repeats (私人处方与重复配药)
Repeatable Prescriptions (可重复处方)
- NHS Prescriptions: Generally not repeatable (unless on the specific “Electronic Repeat Dispensing” service).
- Private Prescriptions: Can be repeated only if directed by the prescriber.
- Instruction: “Repeat x 2” means dispense the original + 2 repeats = 3 total supplies.
- Oral Contraceptives Exception: Historically, if a private Rx for the Pill did not specify repeats, pharmacists could repeat it 5 times (6 total) within 6 months. However, strict modern interpretation usually requires explicit instruction.
Record Keeping (记录保存)
- Private Rx: Must be retained for 2 years from the date of the last supply.
- POM Register: Private prescriptions for POMs must be recorded in the POM register (entry made within 24 hours).
5. Veterinary Prescriptions (兽医处方)
-
Statement: Must clearly state “For animal treatment only” (仅限动物治疗).
-
Prescriber: Veterinary Surgeon.
-
The Cascade (级联系统):
- Licensed veterinary medicine.
- Licensed human medicine (Off-label use).
- Extemporaneous preparation.
- Note: Pharmacists can supply human medicines for animals if prescribed by a vet under the cascade.
-
Physical Presence: The animal does not need to be present in the pharmacy.
Summary Checklist (考试速记)
| Scenario | Legal Status | Action |
|---|---|---|
| Faxed Rx | Not Valid | Treat as Emergency Supply (Dr request). Hard copy in 72h. |
| EEA Doctor Rx (Amoxicillin) | Valid | Dispense. |
| EEA Doctor Rx (Tramadol) | Invalid | Do NOT Dispense (Tramadol is CD Sch 3). |
| EEA Doctor Rx (Diazepam) | Valid | Dispense (Diazepam is CD Sch 4). |
| Emergency Supply (Patient) - Morphine | Illegal | Never supply Sch 2 CDs emergently. |
| Emergency Supply (Patient) - Phenobarbital | Legal | Epilepsy exception. Max 5 days. |
| Emergency Supply (Patient) - Ramipril | Legal | Max 30 days. |
LECTURE29 01 Core Concept 26 Introduction to management planning
Core Concept: Management is the process of getting things done through others. Planning is the foundational function of management.
1. What is Management? (什么是管理)
Henri Fayol’s 5 Functions of Management (法约尔的五大管理职能)
Henri Fayol (1916) defined management as:
- Planning (计划): Predicting the future and drawing up a plan of action. “To foresee and provide means.”
- Organising (组织): Mobilising material and human resources.
- Commanding (指挥): Leading people to achieve goals.
- Coordinating (协调): Unifying and harmonising all activities and efforts.
- Controlling (控制): Seeing that everything occurs in conformity with the established rule and command.
Efficiency vs. Effectiveness (彼得·德鲁克)
- Efficiency (效率): Doing things right (Process-focused).
- Effectiveness (效能): Doing the right things (Outcome-focused).
- Goal: Managers usually aim to be efficient, but effectiveness is often more critical for leadership.
2. The Planning Hierarchy (规划层级)
Planning is not “one size fits all.” It happens at three distinct levels:
1. Strategic Planning (战略规划)
- Scope: Long-term (3–5+ years).
- Focus: The “Big Picture.” Defines the organization’s mission, vision, and long-term goals.
- Who: Top Management (Board, CEO).
- Example: “We want to become the leading cancer research hospital in the UK.”
2. Tactical Planning (战术规划)
- Scope: Mid-term (1–3 years).
- Focus: Implementation. Breaking down strategic goals into specific departmental actions.
- Who: Middle Management.
- Example: “The Pharmacy Department will implement a new aseptic compounding unit by next year.”
3. Operational Planning (运营规划)
- Scope: Short-term (Daily/Weekly/Monthly).
- Focus: Day-to-day processes and routine tasks.
- Who: Front-line Managers / Supervisors.
- Example: “Staff rostering for next week,” “Ordering stock for the weekend.”
3. Mission vs. Vision (使命与愿景)
- Mission Statement (使命):
- Defines the present state.
- Answers: “What do we do? Who do we serve? How do we serve them?”
- Example: “To provide high-quality pharmaceutical care to our local community.”
- Vision Statement (愿景):
- Defines the future state.
- Answers: “Where do we want to be? What does success look like?”
- Example: “To be the world’s most trusted healthcare partner.”
4. Strategic Analysis Tools (战略分析工具)
Before planning, you must analyse the environment.
A. PESTLE Analysis (External Environment)
Used to scan the macro-environment (external factors you cannot control but must adapt to).
| Letter | Factor | Examples in Pharmacy |
|---|---|---|
| P | Political | NHS funding changes, Brexit implications, Trade tariffs. |
| E | Economic | Inflation rates, drug pricing, exchange rates (importing drugs). |
| S | Social | Ageing population, increasing demand for home-care, public health trends. |
| T | Technological | Electronic prescribing (EPS), robotic dispensing, AI diagnosis. |
| L | Legal | Medicines Act, GPhC regulations, Health & Safety laws. |
| E | Environmental | Carbon footprint of inhalers, waste disposal regulations. |
B. SWOT Analysis (Internal & External)
Used to analyse the specific organization.
- Internal Factors (You can control):
- Strengths (S): What do you do well? (e.g., “Highly trained staff,” “Good location”).
- Weaknesses (W): Where are you lacking? (e.g., “Outdated IT system,” “Staff shortages”).
- External Factors (You cannot control):
- Opportunities (O): What market trends can you exploit? (e.g., “New Pharmacy First service launched”).
- Threats (T): What external forces could harm you? (e.g., “Competitor opening next door,” “Drug shortages”).
5. Setting Objectives: SMART Goals (设定目标)
Once the analysis is done, you set objectives. Vague goals like “Improve service” fail. Goals must be SMART:
- S - Specific (具体): Clear and unambiguous.
- Bad: “Improve dispensing.”
- Good: “Reduce dispensing errors.”
- M - Measurable (可衡量): Must have a metric.
- Good: “Reduce dispensing errors by 50%.”
- A - Achievable (可实现): Realistic given resources.
- R - Relevant (相关): Aligns with the broader mission.
- T - Time-bound (有时限): Has a deadline.
- Final Goal: “Reduce dispensing errors by 50% within the next 6 months.”
Summary Checklist (复习清单)
- [ ] Management Functions: Planning, Organising, Commanding, Coordinating, Controlling (Henri Fayol).
- [ ] Planning Levels: Strategic (Long) $\rightarrow$ Tactical (Medium) $\rightarrow$ Operational (Short).
- [ ] PESTLE: Used for External Macro-environmental analysis.
- [ ] SWOT: Internal (Strengths/Weaknesses) + External (Opportunities/Threats).
- [ ] SMART: Specific, Measurable, Achievable, Relevant, Time-bound.
LECTURE30 01 Audit, Evaluation and Research
Lecturer: [Name not explicitly stated in text, likely Course Lead]
1. Context: Clinical Governance (临床治理)
- Definition: A framework through which NHS organisations are accountable for continually improving the quality of their services and safeguarding high standards of care.
- Key Pillars: Education, Clinical Audit, Clinical Effectiveness, Risk Management, Research and Development.
- Relevance: Pharmacists use AER (Audit, Evaluation, Research) tools to measure and improve patient outcomes within this framework.
2. The “AER” Distinction (核心区别)
It is critical to distinguish between these three because they have different ethical requirements and regulatory frameworks (e.g., NHS REC approval).
A. Research (研究)
- Goal: To generate new knowledge or test a hypothesis.
- Key Question: “What is the right thing to do?” (finding out something unknown).
- Characteristics:
- Often involves randomisation (allocating patients to different treatments).
- Results are intended to be generalisable (applicable to other hospitals/populations).
- Requires strict Research Ethics Committee (REC) approval.
B. Clinical Audit (临床审计)
- Goal: To measure practice against a pre-existing standard.
- Key Question: “Are we doing the right thing?” (Checking compliance with guidelines).
- Characteristics:
- Does not involve randomisation or changing treatment; it observes current practice.
- Aims to inform local decision-making and quality improvement, not necessarily generalisable.
- Usually does not require Research Ethics approval (institutional approval is sufficient).
C. Service Evaluation (服务评估)
- Goal: To judge a current service to aid local decision-making.
- Key Question: “What standard does this service achieve?”.
- Characteristics:
- Measures current care without reference to a strict external standard (unlike Audit).
- No randomisation.
- Results are specific to the local setting.
3. Comparison Table: Determining the Project Type
| Feature | Research (研究) | Clinical Audit (临床审计) | Service Evaluation (服务评估) |
|---|---|---|---|
| Intent | Generate new knowledge | Improve quality of care against a standard | Judge current service |
| Treatment | May involve experimental protocol/placebo | Routine clinical care (no change) | Routine clinical care |
| Allocation | Randomisation possible | No randomisation | No randomisation |
| Analysis | Statistical testing to prove hypothesis | Comparison against target (e.g., “90% compliance”) | Descriptive analysis |
| Generalisability | Yes (Universal application) | No (Local application) | No (Local application) |
| Ethics Approval | Required (NHS REC) | Not usually required (Hospital governance) | Not usually required |
4. The Clinical Audit Cycle (临床审计循环)
Audit is not just data collection; it is a cyclical process of improvement.
- Select Topic: Choose a high-risk, high-volume, or high-cost area (e.g., Antibiotic prescribing).
- Agree Standards: Define criteria based on guidelines (e.g., NICE guidelines).
- Example: “100% of patients with community-acquired pneumonia should receive antibiotics within 4 hours.”
- Collect Data: Retrospective (looking back) or Prospective (going forward).
- Analyse Results: Compare actual practice vs. the standard.
- Implement Change: Crucial step. Education, new protocols, system changes.
- Re-audit: Repeat the cycle to confirm improvement.
Donabedian’s Model: Audit can look at Structure (resources), Process (what we do), or Outcome (impact on health).
5. Governance and Ethics (治理与伦理)
HRA Decision Tool (HRA 决策工具)
- The Health Research Authority (HRA) provides an online decision tool to help you determine if your project is “Research”.
- Key Criterion: If you are randomising patients or using a protocol that changes their care, it is likely Research.
Ethics Committees
- NHS REC (Research Ethics Committee): Required if your research involves NHS patients, tissue, or data.
- UREC (University Research Ethics Committee): Required for university research involving healthy volunteers or students.
- Governance: Even Audits need “Governance approval” from the hospital (e.g., Caldicott Guardian for data protection), even if they don’t need ethical approval.
6. Summary Checklist (复习清单)
| Concept | Description |
|---|---|
| Is it Research? | Check: Is there randomisation? Is it generalisable? Is it creating new knowledge? |
| Is it Audit? | Check: Are you comparing against a known standard (e.g., NICE)? |
| Is it Evaluation? | Check: Are you just asking “how is this service running?” without a standard? |
| HRA Tool | The definitive online tool to check if you need NHS ethics approval. |
LECTURE34 01 Core Concept 30 Stages of change cycle
Model: Transtheoretical Model (跨理论模型)
Origin: Developed by Prochaska & DiClemente (1983), originally for smoking cessation.
Core Concept: Behaviour change is not a single event, but a Cyclical Process (循环过程). People move through specific stages and often spiral through them multiple times before achieving permanent change.
1. The 6 Stages of Change (改变的六个阶段)
Stage 1: Pre-contemplation (前意向期 / 无意图期)
- Definition: The patient has no intention to take action in the foreseeable future (typically defined as the next 6 months).
- Patient Mindset:
- “Happy User” (快乐的使用者): They don’t see their behaviour as a problem (Denial).
- Unaware (无意识): Lack information about the consequences.
- Demoralised (泄气): May have tried before and failed, giving up hope.
- Pharmacist’s Role:
- Raise Awareness (提高意识): Provide non-judgmental information.
- Personalise Risks (个性化风险): Link the behaviour to their specific symptoms (e.g., cough, cost).
- Goal: Move them to thinking about it. Don’t push too hard or nag.
Stage 2: Contemplation (意向期 / 沉思期)
- Definition: The patient is aware that a problem exists and is seriously thinking about overcoming it, but has not yet made a commitment (usually within the next 6 months).
- Patient Mindset:
- Ambivalence (矛盾心理): This is the key characteristic. They are “sitting on the fence”.
- Weighing Pros & Cons: They know what they should do, but are attached to what they want to do.
- Can get stuck here for a long time (“Chronic Contemplation”).
- Pharmacist’s Role:
- Tip the Balance (打破平衡): Help them see that the Benefits of Change > Costs of Change.
- Motivate (激励): Identify their personal motivators and barriers.
Stage 3: Preparation (准备期)
- Definition: The patient intends to take action in the immediate future (usually within the next month).
- Patient Mindset:
- They are ready to act.
- May have taken small steps (e.g., bought nicotine patches, joined a gym, cut down cigarette numbers).
- Pharmacist’s Role:
- Goal Setting (设定目标): Help them set a specific “Quit Date” or start date.
- Action Plan (行动计划): Discuss suitable therapies (NRT, Varenicline) and strategies.
- Encourage (鼓励): Reinforce their decision.
Stage 4: Action (行动期)
- Definition: The patient has made specific, overt modifications in their lifestyle within the past 6 months.
- Patient Mindset:
- This is the busiest stage requiring the most energy and commitment.
- They are actively “doing” the change (e.g., not smoking).
- High risk of relapse during this phase.
- Pharmacist’s Role:
- Support (支持): Ensure they use medication correctly (e.g., NRT technique).
- Problem Solving (解决问题): Help manage Withdrawal Symptoms (戒断症状) or side effects.
- Positive Reinforcement (正向强化): Praise their success to build Self-Efficacy (自我效能).
Stage 5: Maintenance (维持期)
- Definition: The patient is working to prevent relapse and consolidate the gains.
- Patient Mindset:
- Typically defined as from 6 months to 5 years.
- They are more confident, and the behaviour is becoming a habit.
- Temptation is reduced but not gone.
- Pharmacist’s Role:
- Relapse Prevention (复发预防): Identify “danger situations” (triggers like stress, parties) and plan coping strategies.
Stage 6: Relapse (复发)
- Definition: Regression to an earlier stage (usually Pre-contemplation or Contemplation).
- Core Concept: Relapse is the rule, not the exception. It is part of the cycle.
- Patient Mindset:
- May feel guilty, like a failure, or demoralised.
- Pharmacist’s Role:
- Non-judgmental Support (非评判性支持): “Don’t beat yourself up.”
- Learning Opportunity (学习机会): “What caused the slip? What can we do differently next time?”
- Re-engage (重新参与): Encourage them to enter the preparation stage again immediately.
2. Summary Table (考试速记表)
| Stage (阶段) | Key Characteristic (关键特征) | Pharmacist Strategy (策略) |
|---|---|---|
| Pre-contemplation | No intention (Happy user / Denial) | Educate & Personalise risks. |
| Contemplation | Ambivalence (Sitting on the fence) | Motivate & Tip the balance (Pros > Cons). |
| Preparation | Planning (Ready in < 1 month) | Set a Date & Discuss Treatment. |
| Action | < 6 months since change | Support, Manage Withdrawal, Reward. |
| Maintenance | > 6 months since change | Prevent Relapse & Coping Strategies. |
| Relapse | Slip back (Common event) | Re-frame as learning & Re-engage. |
LECTURE38 01 Core Concept 34 Interactive Law Revision Session
Lecturer: Professor Ellen Schafheutle
Focus: GPhC Registration Assessment Style Questions (Closed book scenarios).
Core Topic: Application of the Medicines Act and Human Medicines Regulations in practice.
1. Medicines Classification & Sales (药品分类与销售)
Paracetamol Quantity Rules (扑热息痛销售数量规则)
Scenario: What is the maximum number of Paracetamol 500mg capsules/tablets that can be legally sold from a pharmacy without a prescription?
- Legal Limit (法律上限): 100 capsules/tablets.
- Explanation:
- GSL (General Sales List - 一般清单药物): Standard packs are usually 16 or 32.
- P Medicine (Pharmacy Only - 药房专售药物): You can sell packs larger than 32, up to 99.
- POM Threshold (处方药门槛): If the quantity is > 100 (for non-effervescent tablets), it becomes a Prescription Only Medicine (POM).
- Note: While selling 100 is legal (e.g., 3 packs of 32), you must use Professional Judgment (职业判断) to ensure safety and prevent overdose.
Responsible Pharmacist (RP) Absence (责任药师缺席)
Scenario: The Responsible Pharmacist (RP) has signed in but is physically absent (e.g., at lunch) for less than 2 hours. No other pharmacist is present.
- Allowed Transactions (允许的交易):
- Sale of GSL medicines (销售GSL药物): YES. Permitted if a protocol is in place and staff are trained.
- Prohibited Transactions (禁止的交易):
- Sale of P medicines (销售P类药物): NO. Requires pharmacist supervision.
- Supply of Prescribed Medicines (Handing out dispensed meds): NO. Even if bagged and ready, they cannot be handed out without the RP present.
2. Prescribers & Prescriptions (处方医师与处方)
Appropriate Practitioners (合法的处方医师)
Who can prescribe POMs?
- Doctors (医生): All registered doctors (GMC).
- Dentists (牙医): All registered dentists (GDC).
- Restriction: Must prescribe only for conditions relevant to dental practice (牙科执业范围).
- Pharmacists / Nurses: NOT all. Only those qualified as Independent Prescribers (IP - 独立处方医师) or Supplementary Prescribers.
- Optometrists (验光师): Only if qualified as IPs.
Prescription Requirements (处方要求)
A valid paper prescription for a POM must include:
- Signature (签名): In ink by the prescriber.
- Date (日期): Valid for 6 months (28 days for Schedule 2, 3, 4 CDs).
- Prescriber’s Address (医师地址): Must be in the UK.
- Patient’s Name & Address (患者姓名与地址).
- Medicine Details: Name, Formulation, Strength.
- Note on Dose: For standard POMs, specific directions (e.g., “One daily”) are required by good practice, but legally “As directed” is sometimes accepted (though Illegal for CDs).
- Note on Age: Patient’s age/DOB is NOT legally required on a standard POM prescription unless the patient is under 12 years old (12岁以下).
3. Emergency Supply (紧急供应)
The “Interview” Requirement (面谈要求)
Scenario: A mother asks for an emergency supply of medication for her 17-year-old son. The son is not present. She says he has run out and needs it urgently.
- Legal Status: Providing the supply to the mother based only on her request is ILLEGAL (违法).
- Reasoning:
- The law requires the pharmacist to “Interview the patient” (与患者面谈).
- Exceptions: Unless it is “impracticable” to do so (e.g., the patient is a very young child or severely mentally/physically disabled).
- Analysis: A 17-year-old is generally considered competent. The pharmacist must speak to the son (e.g., via telephone) to satisfy the “interview” requirement before supplying the medication to the mother.
Age Restrictions?
- There is no specific legal age limit (like 18+) for receiving an emergency supply. It depends on the patient’s competence and the pharmacist’s professional judgment.
4. Professional Judgment (职业判断)
Question: When faced with an ethical dilemma where the law is permissive but safety is a concern, or the law is strict but patient harm is imminent, what must a pharmacist do?
- Action:
- Use Professional Judgment (职业判断) to decide the most appropriate course of action.
- Be able to Justify (证明/辩护) the decision to Peers (同行).
- Note: You do not need to check with insurance companies first; they deal with liability after events, not clinical decisions during events.
Summary Checklist for Exams (考试速记)
| Topic | Rule | Note |
|---|---|---|
| Paracetamol Limit | 100 (Legal sale limit) | >100 is POM. |
| RP Absence | GSL Only | No P meds, No handing out prescriptions. |
| Dentist Rx | Valid for POMs | Restricted to dental use (e.g., Antibiotics, Fluoride). |
| Emergency Supply | Interview Patient | Mandatory unless strictly impracticable. Parents cannot request for competent teenagers without the teen’s involvement. |
| Rx Date | 6 Months | Standard POMs. |

